ENT
A Case Report of Facial Swelling and Crepitus Following a Dental Procedure
DOI: https://doi.org/10.21980/J83W8HGiven the physical exam findings of crepitus on the right neck up to the right lower eyelid, a maxillofacial CT scan without contrast was performed. It revealed diffuse subcutaneous air within the soft tissues of the face and neck and free air within the pre-septal soft tissue of the right eye, appearing as hyperlucent (dark) areas on CT within the soft tissue planes (blue outline). It showed no evidence of post-septal free air. A single-view chest X-ray was also performed and was unremarkable except for incompletely imaged soft tissue gas in the right lower neck (blue outline). On flexible fiberoptic laryngoscopy performed by ENT, the oropharynx appeared diffusely edematous and narrowed.
Case Report of Post-Operative Uvular Necrosis Following Intubation
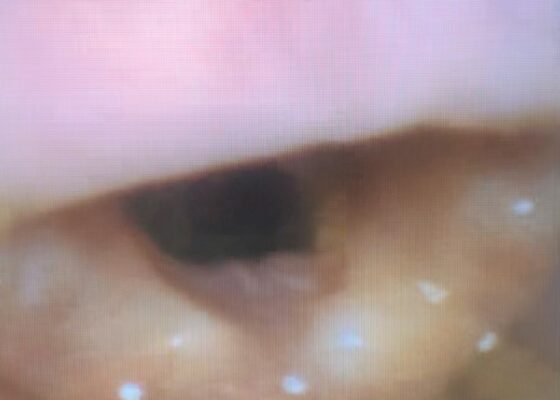
DOI: https://doi.org/10.21980/J8065JThe distal portion of her uvula was necrotic with a clear demarcation approximately halfway up the uvula. She had no trauma to the anterior oropharyngeal structures, tonsils, or adenoids. There were no lesions to the hard or soft palate. She had no carotid bruits or thrills, and no tenderness over the anterior portion of the neck.
Retropharyngeal Abscess in an Adult Patient Presenting with Neck Fullness and Dysphagia: A Case Report
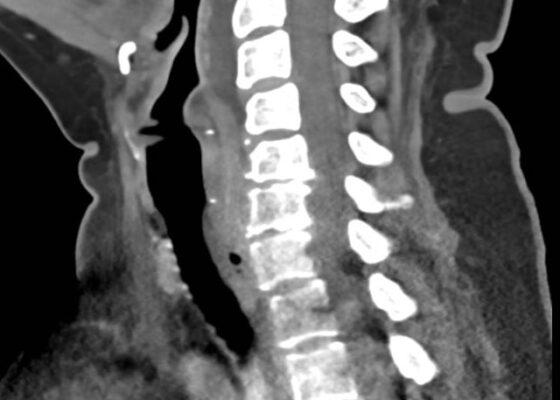
DOI: https://doi.org/10.21980/J8M36GContrast-enhanced CT soft tissue of the neck showed evidence of a prevertebral/retropharyngeal fluid collection, extending from the odontoid tip to the inferior C4 vertebral body margin, measuring 5.4 x 1.0 x 3.3 centimeters (cm) in size (yellow lines) without gross airway narrowing.
The Advantage of Using Video Laryngoscope in Puncture and Incisional Drainage of Peritonsillar Abscess: A Case Report
DOI: https://doi.org/10.21980/J8G935Incision of the peritonsillar abscess was performed with the assistance of the C-MAC video laryngoscope which provided a clear, illuminated, and unobstructed view of the incision site. Local anesthesia with 1% xylocaine was administered, and the abscess was incised with a scalpel and drained with a forceps.
A Man with Sore Throat—A Case Report
DOI: https://doi.org/10.21980/J8MH0BVideo laryngoscopy of the upper airway was performed two days after initial burn injury. The images obtained demonstrated laryngeal edema and inflammation near the epiglottis. The dot identifies the epiglottis and the asterix identifies the area of moderate thermal burns. Imaging also demonstrated adequate patency of airway and ruled out the need for intubation at that time.
Evaluation of ACE-inhibitor Induced Laryngeal Edema Using Fiberoptic Scope: A Case Report
DOI: https://doi.org/10.21980/J83P9TPhysical exam was initially significant for swelling isolated to the right sided cheek and upper lip. There was no edema to lower lip, uvular swelling, or swelling to the submandibular space. She was speaking full sentences and did not endorse any voice changes. Initial vital signs were as follows: BP 125/77, HR 74, RR 16, and oxygen saturation of 100% on room air. Approximately 40 minutes later, after 125 mg solumedrol intravenous (IV) and 50mg diphenhydramine by mouth, swelling had spread to the entire upper lip and the patient reported spreading to her jaw (Photo 1). Although no jaw or submandibular edema was appreciated on physical exam, a flexible fiberoptic laryngoscope was used to evaluate the patient’s airways given worsening symptoms. Viscous lidocaine was applied intranasally five minutes prior to the procedure. The patient was positioned in a seated position on the stretcher. A flexible fiberoptic laryngoscope was then inserted through the nares and advanced slowly. Laryngoscopy showed diffuse edema of the epiglottis, arytenoids, and ventricular folds (see photos 2-4). Vital signs and respiratory status remained stable both during and after the procedure.
Peritonsillar Abscess Simulator: A Low-Cost, High-Fidelity Trainer
DOI: https://doi.org/10.21980/J85M0BBy the end of this training session, learners will be able to: 1) locate the abscess, 2) perform needle aspiration, and 3) develop dexterity in maneuvering instruments in the small three-dimensional confines of the oral cavity without causing injury to local structures.
A Case Report of Epiglottitis in an Adult Patient
DOI: https://doi.org/10.21980/J8QM09At the time of presentation to the ED, laboratory results were significant for leukocytosis to 11.8 x 109 white blood cells/L and a partial pressure of carbon dioxide of 52 mmHg on venous blood gas. Computed tomography (CT) of the soft tissue of the neck with contrast showed edematous swelling of the epiglottis and aryepiglottic fold with internal foci of gas (blue arrow) and partial effacement of the laryngopharyngeal airway and scattered cervical lymph nodes bilaterally (Figure 1). Findings were consistent with epiglottitis containing nonspecific air. Additionally, the pathognomonic “thumbprint sign” (yellow arrow) was found on lateral x-ray of the neck (Figure 2). The CT findings as shown in figure 3 illustrate lateral view of the swelling of the epiglottis, gas, and blockage of the airway.