Abdominal/Gastroenterology
Procedural Sedation for the removal of a rectal foreign body
DOI: https://doi.org/10.21980/J81332Axial and coronal views on CT showed evidence of a large, tube-shaped foreign body in the rectum (see arrows) without evidence of acute gastrointestinal tract disease.
Large Ventral Hernia
DOI: https://doi.org/10.21980/J86K9QComputed tomography (CT) scan with intravenous (IV) contrast of the abdomen and pelvis demonstrated a large pannus containing a ventral hernia with abdominal contents extending below the knees (white circle), elongation of mesenteric vessels to accommodate abdominal contents outside of the abdomen (white arrow) and air fluid levels (white arrow) indicating a small bowel obstruction.
Elderly female with acute abdominal pain presenting with Superior Mesenteric Artery Thrombus
DOI: https://doi.org/10.21980/J82W52Computed tomography (CT) angiogram of the abdomen and pelvis revealed a superior mesenteric artery (SMA) thrombosis 5 cm from the origin off of the abdominal aorta. As seen in the sagittal view, there does not appear to be any contrast 5 cm past the origin of the SMA. On the axial views, you can trace the SMA until the point that there is no longer any contrast visible which indicates the start of the thrombus. The SMA does not appear to be reconstituted. There was normal flow to the celiac artery. (See annotated images).
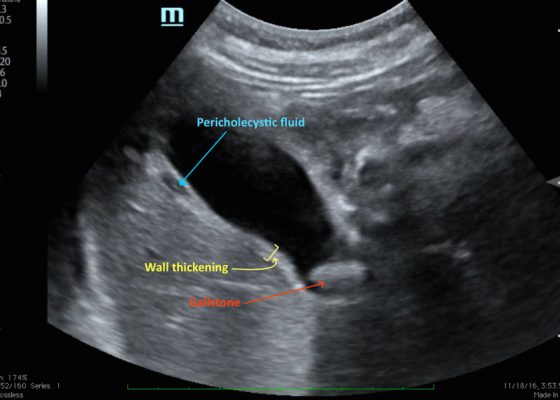
A Case of Acute Cholecystitis
DOI: https://doi.org/10.21980/J8405QBedside point-of-care ultrasound revealed a distended gallbladder, thickened gallbladder wall, pericholecystic fluid, and a stone in the neck of the gallbladder indicative of acute cholecystitis.
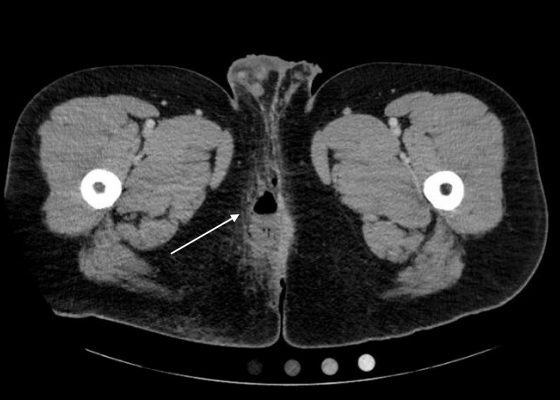
Perianal Abscess
DOI: https://doi.org/10.21980/J8QP81Computed Tomography (CT) of the Pelvis with intravenous (IV) contrast revealed a 5.7 cm x 2.4 cm air-fluid collection in the right perianal soft tissue along the right gluteal cleft, with surrounding fat stranding, consistent with a perianal abscess with cellulitis.
An Elderly Male with Amyand’s Hernia
DOI: https://doi.org/10.21980/J80D13Ultrasound of the right scrotum shows a right inguinal hernia with an air-containing loop of bowel (white arrow) and a non-compressible appendix (yellow arrow). Coronal and axial views of abdomen-pelvis CT show a right inguinal hernia containing a loop of small bowel (white arrow) and appendix (yellow arrow).
Pediatric Esophageal Foreign Body
DOI: https://doi.org/10.21980/J8GD1FA radiopaque foreign body was visualized in the proximal esophagus at the thoracic inlet on the chest and neck radiographs. The foreign body appeared to be metallic with visualized concentric rings consistent with a coin.
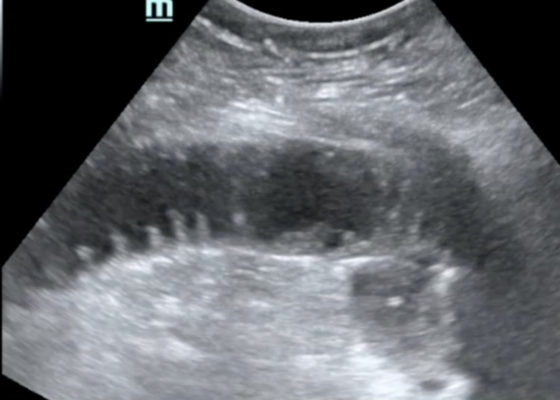
Bedside Ultrasound for the Diagnosis of Small Bowel Obstruction
DOI: https://doi.org/10.21980/J86W6PThe POCUS utilizing the low frequency curvilinear probe demonstrates fluid-filled, dilated bowel loops greater than 2.5cm with to-and-fro peristalsis, and thickened bowel walls greater than 3mm, concerning for SBO.