Posterior Vitreous Detachment
History of present illness:
Patient is a 41-year-old female without previous ophthalmologic disease who presented to emergency department with a one-day history of painless visual changes. She described seeing shadows and floaters in the lower visual field of her right eye and denied flashes of light or complete darkness in that field. Physical exam indicated visual acuity 20/20 in left eye and 20/20 in right eye with vision grossly intact other than chief complaint. There were no signs of facial or head trauma; extra-ocular movements were intact with pupils equal, round, and reactive.
Significant findings:
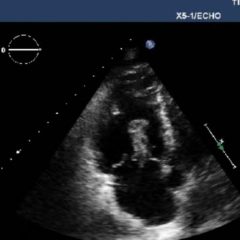
Ocular ultrasound was performed and demonstrated a thin, slightly echogenic strand (blue arrow) extending from the posterior eye into the vitreous humor (yellow arrow) which was hyperkinetic with extraocular motion. These findings are consistent with a posterior vitreous detachment (PVD).
Discussion:
Posterior vitreous detachment is the dehiscence of the vitreous membrane from the surface of the retina. Cataract surgery and age greater than 70 are the most common risk factors for PVD, although it can occur at any age.1 The symptoms of PVD can mimic a more serious retinal detachment (RD) in visual field defects or flashing/flickering lights.2 Patients presenting with these symptoms usually have a benign etiology; however, 10%–26% will have a more serious retinal disease including RD and retinal tear.3,4,5,6
Retinal detachment presents in ocular ultrasound as a taut, hyperechoic strand that moves in conjunction with extraocular movement. Posterior vitreous detachment presents as a much thinner and less echogenic strand that is hyperkinetic and wave-like with extraocular movement, described as swaying seaweed in appearance.6,7,8,9
Multiple studies affirmed the ability of emergency physicians to reliably diagnose RD,10,11 and overall vitreoretinal disease (defined as RD, PVD, and vitreous hemorrhage).9 However, emergency physicians are only moderately successful at differentiating RD vs. PVD, identifying RD 74.6% of the time and PVD 85.7% of the time.7 As a result, it is important to note a key differentiating factor on ultrasound: a RD will be attached to the optic nerve sheath, while a PVD will not, crossing the area of the optic nerve.
Posterior vitreous detachment is not a sight-threatening emergency and therefore does not necessitate an emergent ophthalmology consultation. Most people develop PVD at some point in their lives and the vast majority have a benign course with no treatment and without complications.4However a delay in the diagnosis of RD can lead to irreversible loss of vision.7,11 Therefore it is important for emergency physicians to be able to differentiate between the two with point-of-care ocular ultrasound.
This patient was seen in the ophthalmology office within one day for follow up. Fortunately for this patient, as with most cases of PVD, immediate treatment was not indicated.
Topics:
Ultrasound, ophthalmology, posterior vitreous detachment.
References:
- Ivastinovic D, Schwab C, Borkenstein A, Lackner EM, Wedrich A, Velikay-parel M. Evolution of early changes at the vitreoretinal interface after cataract surgery determined by optical coherence tomography and ultrasonography. Am J Ophthalmol. 2012;153(4):705-709. doi: 10.1016/j.ajo.2011.09.009.
- Schott ML, Pierog JE, Williams SR. Pitfalls in the use of ocular ultrasound for evaluation of acute vision loss. J Emerg Med. 2013;44(6):1136-1139. doi: 10.1016/j.jemermed.2012.11.079.
- Dayan MR, Jayamanne DG, Andrews RM, Griffiths PG. Flashes and floaters as predictors of vitreoretinal pathology: is follow-up necessary for posterior vitreous detachment? Eye (Lond).1996;10(4):456-458. doi: 1038/eye.1996.100.
- Hollands H, Johnson D, Brox AC, Almeida D, Simel DL, Sharma S. Acute-onset floaters and flashes: is this patient at risk for retinal detachment? JAMA. 2009;302(20):2243-2249. doi: 10.1001/jama.2009.1714.
- Mitry D, Charteris DG, Fleck BW, Campbell H, Singh J. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010;94(6):678-684. doi: 10.1136/bjo.2009.157727.
- Woo MY, Hecht N, Hurley B, Stitt D, Thiruganasambandamoorthy V. Test characteristics of point-of-care ultrasonography for the diagnosis of acute posterior ocular pathology. Can J Ophthalmol. 2016;51(5):336-341. doi: 10.1016/j.jcjo.2016.03.020.
- Baker N, Amini R, Situ-lacasse EH, et al. Can emergency physicians accurately distinguish retinal detachment from posterior vitreous detachment with point-of-care ocular ultrasound? Am J Emerg Med. 2018;36(5):774-776. doi: 10.1016/j.ajem.2017.10.010.
- Riaz A, Shah C, Wei G. Retinal detachment. J Educ Teach Emerg Med. 2018;3(2): V6-V7. doi:10.21980/j8204q.
- Shinar Z, Chan L, Orlinsky M. Use of ocular ultrasound for the evaluation of retinal detachment. J Emerg Med. 2011;40(1):53-57. doi: 10.1016/j.jemermed.2009.06.001.
- Blaivas M, Theodoro D, Sierzenski PR. A study of bedside ocular ultrasonography in the emergency department. Acad Emerg Med. 2002;9(8):791-799.
- Yoonessi R, Hussain A, Jang TB. Bedside ocular ultrasound for the detection of retinal detachment in the emergency department. Acad Emerg Med. 2010;17(9):913-917. doi: 10.1111/j.1553-2712.2010.00809.x.