Re-expansion Pulmonary Edema
History of present illness:
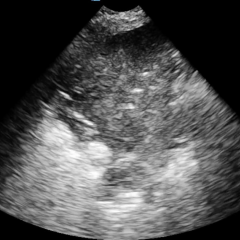
A 95-year-old male with history of atrial fibrillation presented to the emergency department for shortness of breath for one week. A chest X-ray showed a large right-sided pleural effusion. Given the unknown etiology of the effusion, and the patient’s dyspnea, a thoracentesis was performed. Under ultrasound guidance, 2.9 liters of cloudy yellow fluid was removed. The patient tolerated the procedure well and a post procedural chest X-ray was performed, which is noted below. A few hours later, the patient became tachypneic and oxygenation saturation dropped from 100% to 91%-92% on room air, and was found to have decreased breath sounds on the right. An additional chest X-ray was performed which showed pulmonary re-expansion edema and patient was subsequently admitted for observation.
Significant findings:
Initial chest X-ray (chest X-ray 1) showed a right-sided pleural effusion with compressive atelectasis of the mid to lower right lung. Repeat chest X-ray immediately after evacuation (chest X-ray 2) shows improvement of the pleural effusion and a new trace apical right pneumothorax measuring 6.7 mm. When the patient became tachypneic, a third X-ray (chest X-ray 3) showed persistent trace apical right pneumothorax measuring 6.7 mm.
Discussion:
Re-expansion pulmonary edema (RPE) is a rare complication that can occur following thoracentesis of a pleural effusion or chest tube drainage of pneumothorax, and is a potentially fatal complication due to the resulting abrupt reduction in pleural pressure.1,2 RPE pathophysiology is not fully understood; however, risk factors include presence of pleural effusion in conjunction with pneumothorax, young patients (<40), large pneumothoraces, and when pneumothorax has been present for longer than one week.3 Large volume thoracenteses are characterized by removal of more than 1000 mL of pleural fluid during a therapeutic thoracentesis.4
It is important to note that RPE is usually self-limiting and treatment is generally supportive, typically ranging from oxygen support and diuretics to intubation, mechanical ventilation, hemodynamics, and steroids in more severe cases.1,5 Preventive strategies include limiting drainage of pleural fluid if the patient reports chest pressure or discomfort during thoracentesis and using low negative pressure (less than −20 cm H2O) for suction.6 A more precise treatment approach may establish a “safe” volume of fluid to remove by combining symptom monitoring with serial measures of pleural pressure. Using this methodology, the amount of fluid aspirated often exceeds the traditionally observed limits of 1000 to 1500 mL, and many patients fare well with removal above 1500 mL.4 As with traditional methods of therapeutic thoracentesis, precautions are followed and fluid removal is stopped if the patient feels chest pressure or becomes hypotensive, if pleural pressure falls less than -20 cm H2O, or if no more fluid can be aspirated.4 Close patient monitoring and early recognition of symptoms, especially in the presence of known risk factors, is paramount because delayed treatment may lead to a fatal outcome.
Topics:
Re-expansion pulmonary edema, pleural effusion, thoracentesis, pneumothorax, drainage, chest tube, ventilation.
References:
- Meeker J, Jaeger A, Tillis W. An uncommon complication of a common clinical scenario: exploring reexpansion pulmonary edema with a case report and literature review. J Community Hosp Intern Med Perspect. 2016;6(3):10.3402/jchimp.v6.32257. doi: 10.3402/jchimp.v6.32257
- Dias OM, Teixeria LR, Vargas FS. Reexpansion pulmonary edema after therapeutic thoracentesis. Clinics. 2010;65(12):1387-1389. doi: 10.1590/S1807-59322010001200026
- Echevarria C, Twomey D, Dunning J, Chanda B. Does re‐expansion pulmonary oedema exist? Interact Cardivoasc Thorac Surg. 2008;7:485-489. doi: 10.1510/icvts.2008.178087
- Light RW, Jenkinson SG, Minh VD, George RB. Observations on pleural fluid pressures as fluid is withdrawn during thoracentesis. Am Rev Respir Dis. 1980;121:799-804. doi: 10.1164/arrd.1980.121.5.799
- Verhagen M, Van Buijtenen J, Geeraedts L. Reexpansion pulmonary edema after chest drainage for pneumothorax: a case report and literature overview. Respir Med Case Rep. 2015;14:10-12. doi: 10.1016/j.rmcr.2014.10.002
- Kasmani R, Irani F, Okoli K, Mahajan V. Re-Expansion pulmonary edema following thoracentesis. CMAJ. 2010;182(18): 2000-2002. doi: 10.1503/cmaj.090672