Post-Coital Sudden Cardiac Arrest Due to Non-Traumatic Subarachnoid Hemorrhage—A Case Report
ABSTRACT:
Emergency medicine (EM) learners are taught to approach cardiac arrest algorithmically using Advanced Cardiac Life Support (ACLS) with particular emphasis on treatment. However, when treating patients in cardiac arrest it is important to maintain a broad differential of possible non-cardiac etiologies of the presenting symptoms.
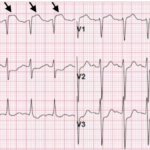
A patient presented to the emergency department (ED) as a post-coital cardiac arrest with prehospital return of spontaneous circulation (ROSC). Electrocardiogram (ECG) suggested a possible coronary artery occlusion. Given the circumstances of the arrest, computed tomography (CT) of the head was performed which demonstrated a large subarachnoid hemorrhage (SAH). Emergent percutaneous coronary intervention (PCI) was deferred due to the alternative explanation for the ECG changes and the patient’s instability. Her condition declined, and soon after the patient expired.
Patients with sudden cardiac arrest (SCA) due to SAH are unlikely to benefit from PCI, hindering a more appropriate workup and treatment.1 When faced with patients presenting with SCA and relevant risk factors, it is important to avoid anchoring bias and consider that the ischemic changes on ECG may not be due to primary cardiac causes.
Topics:
Subarachnoid hemorrhage, sudden cardiac arrest, pulseless electrical activity, ECG, CT.