Radiolucent Foreign Body Seen on Point-of-Care Ultrasound but not on X-ray
History of present illness:
A 35-year-old male patient presented to the emergency department with left foot pain and swelling. He had sustained a puncture wound with a large wood splinter to the lateral aspect of the dorsum of his foot in the week prior. He believed that he had removed the entire splinter, but over the next week, the site became increasingly red, tender, and swollen without drainage.
Significant findings:
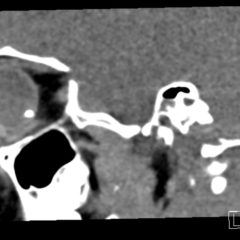
X-rays of the foot were obtained and no radiopaque foreign body was visualized. Due to high clinical suspicion for retained foreign body, a point-of-care ultrasound was performed by applying a high-frequency linear probe at the area of discomfort. In the long axis an ovoid focus of hypoechogenicity (orange outline) is visualized. Within this finding there is a linear focus (yellow line) of increased echogenicity measuring 1 mm in diameter and 1 cm in length. On short axis view, a rectangle focus (green dot) demonstrating shadowing (blue highlight) is seen.
Given the evidence of foreign body on ultrasound, incision and drainage was performed. It resulted in the removal of a 1 cm splinter along with small amount of purulent and serous fluid.
Discussion:
Whenever a patient has a traumatic injury that violates the integrity of the body, there is the possibility of a retained foreign body. It has been reported that missed foreign bodies are the second leading cause of lawsuits in emergency medicine.1 Despite the known risk of litigation, greater than one third of foreign bodies are missed initially on examination.2 This has frequently been attributed to a lack of imaging in conjunction with examination.3 X-rays are thought to be the most common imaging to screen for foreign bodies in extremity trauma.4 Unfortunately, many foreign bodies are not radiopaque on X-ray. Radiopaque foreign bodies are usually more dense than soft tissues and similar to bone density (e.g., metal, stone, or certain types of glass).5 Less dense foreign bodies are radiolucent and not seen on X-ray.
Ultrasound can be superior to X-ray in identifying these foreign bodies: one study showed soft-tissue X-ray had only 10% sensitivity for detection of wood and rubber foreign bodies, with 90% specificity;2 while high-frequency ultrasound had a 90% sensitivity and 80% specificity for these same foreign bodies.Computed tomography and magnetic resonance imaging (MRI) can also potentially identify traditionally radiolucent foreign bodies such as wood. The sensitivity of these modalities depends on the material of the foreign body. For suspected wooden foreign bodies, ultrasound is the favored modality.7
Due to its availability, sensitivity and specificity, ultrasound should be considered in the evaluation of foreign bodies. It can facilitate both the detection and removal of radiolucent foreign bodies.
Topics:
Point-of-care ultrasound, POCUS, radiolucent, radiopaque, X-ray, foreign body, wood foreign body.
References:
- Schlager D. Ultrasound detection of foreign bodies and procedure guidance. Emerg Med Clin North Am. 1997;15(4):895-912. doi: 1016/S0733-8627(05)70338-2
- Jarraya M, Hayashi D, de Villiers RV, et al. Multimodality imaging of foreign bodies of the musculoskeletal system. AJR Am J Roentgenology. 2014;203(1):W92-W102. doi: 10.2214/AJR.13.11743
- Blankenship RB, Baker T. Imaging modalities in wounds and superficial skin infections. Emerg Med Clin North Am. 2007;25(1):223-234. doi: 10.1016/j.emc.2007.01.011
- Broder, J. Imaging the extremities. In: Broder J, ed. Diagnostic Imaging for the Emergency Physician. New York, NY: Elsevier Saunders; 2011:748-846.
- Turkcuer I, Atilla R, Topacoglu H, et al. Do we really need plain and soft-tissue radiographies to detect radiolucent foreign bodies in the ED?Am J Emerg Med. 2006;24(7):763-768. doi: 10.1016/j.ajem.2006.03.013
- Geria R. Ultrasound guided procedures – V. Foreign body localization. Sonoguide. https://www.acep.org/sonoguide/foreign_bodies.html. Accessed October 1, 2018.