Oropharynx Ulceration
History of present illness:
A 31-year-old male presented to the emergency department (ED) with worsening constant left sided throat pain over the past four months. The patient reports that he was brushing his teeth when his dog jumped onto his back causing his toothbrush to puncture the back of his throat, resulting in immediate bleeding and discomfort. The bleeding subsided and the patient did not seek medical care. The pain radiated to his left ear and the back of the neck. He also noted a change in his voice. The day before presenting to the ED the patient noted subjective fevers, hemoptysis and drooling, which led him to seek medical care.
Significant findings:
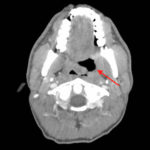
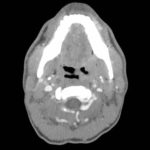
The photograph demonstrates an area of ulcerative tissue at the left palatine tonsil without surrounding erythema or purulent drainage. The computed tomography (CT) scan shows a large ulceration of the left soft palate and palatine tonsil (red arrow). There is no evidence of skull base osteomyelitis. There is suppurative lymphadenopathy with partial left jugular vein compression due to mass effect (yellow highlight). There is mild nasopharyngeal airway narrowing with architectural distortion (blue arrow), but no other evidence of airway obstruction.
Discussion:
The oral cavity is prone to trauma leading to the formation of superficial ulcerations. There are many causes of mechanical trauma, most commonly accidental biting. Chemical, electrical and thermal insults are also possibilities. Poor fitting dental devices and fractured or malformed teeth can also be etiologies.1 Traumatic ulcerations are most common in children given bruxism and thumb sucking. However, a broad differential must be considered including malignant and premalignant lesions, infections of the oral mucosa, aphthous ulcerations and autoimmune diseases.2, 3
Chronic ulcerations are associated with superimposed infection, but there has not been established an association of malignant transformation of the oral mucosa after trauma. If there is an unclear history at presentation, the provider must consider referral for a biopsy to exclude malignancy. Most ulcerations from mechanical or thermal trauma resolve in ten to fourteen days. Antibiotics can be considered to prevent secondary infection if the ulceration is severe; however, most resolve without antibiotics. Supportive measures to consider include removal of irritant, mouth guards, soft diet, sodium chloride mouth rinse, topical corticosteroids or anesthetics. Triamcinolone acetonide and fluocinonide gel are recommended for analgesia.2
The patient discussed here was discharged home after his visit with a plan to follow up for further evaluation by a specialist. He returned to the emergency department three months later with worsening symptoms. He was admitted and otolaryngology performed biopsies, which demonstrated an advanced stage human papillomavirus (HPV) positive oropharyngeal cancer. The patient is currently in a clinical trial receiving treatment. Again, this stresses the importance of follow up and further evaluation of concerning lesions.
Topics:
Oropharynx ulceration, oral lesion, traumatic ulceration, oropharyngeal cancer, HPV, otolaryngology (ENT).
References:
- Gilvettia C, Porter SR, Fedele S. Traumatic and chemical oral ulceration: a case report and review of the literature. Br Dent J.2010;208(7):297-300. doi: 1038/sj.bdj.2010.295
- Field EA, Allan RB. Oral ulceration – aetiopathogenesis, clinical diagnosis and management in the gastrointestinal clinic. Aliment Pharmacol Ther.2003;18(10):949-962. doi: 1046/j.1365-2036.2003.01782.x
- Cunningham S, Quinn F, Ryan M. Ulcerative lesions of the oral cavity. Grand rounds presentation, UTMB, Department of Otolaryngology. https://www.utmb.edu/otoref/grnds/Ulcer-oral-021016/Ulcer-oral-021016.pdf. Presented October 16, 2002. Accessed March 7, 2017.