Archives
The Gravid Watermelon: An Inexpensive Perimortem Caesarean Section Model
DOI: https://doi.org/10.21980/J8705NThe gravid watermelon is a cost-effective model that uses common materials from the supermarket and emergency department (ED), using a carved-out watermelon as a base, representing the peritoneal cavity. Inexpensive respiratory tubing is used to represent intestine; watered down gelatin and a small doll in a deflated rubber/plastic ball is used to represent a gravid uterus. The bladder is represented by an unused, water-filled exam glove, and watermelon pulp represents blood clots and mesentery. The gravid watermelon is covered with an elastic bandage to represent tough muscle and fascia, and topped with a shower curtain for skin.
Low-Cost Portable Suction-Assisted Laryngoscopy Airway Decontamination (SALAD) Simulator for Dynamic Emesis
DOI: https://doi.org/10.21980/J8362BThe economic and dynamic SALAD innovation recreates an actively vomiting patient and replicates visual obstruction from fluid contents during airway management.By the end of the session, learners are expected to: 1) discuss the risks, benefits, indications and contraindications associated with intubation of a vomiting or hemorrhaging patient. 2) Work with colleagues to effectively stabilize a patient who is actively vomiting or bleeding during airway management. 3) Competently perform intubation in the acute setting of visual obstruction from active emesis, hemorrhage, or massive regurgitation. 4) Increase speed and dexterity of intubation by applying the SALAD method when fluid obstructs visualization of the larynx.
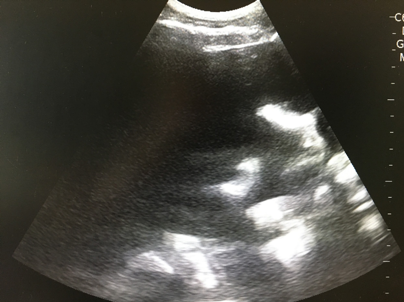
Low-Cost, Low Fidelity Meat Model to Teach Ultrasound Guided Nerve Blocks
DOI: https://doi.org/10.21980/J83G9RUpon completion of this workshop, learners will be able to: 1) Describe the risks and benefits of ultrasound guided nerve blocks. 2) Choose the appropriate nerve to block based on the area that needs anesthesia. 3) Display proficiency in performing an ultrasound guided nerve block on meat models. 4) Verbalize confidence in successfully performing ultrasound guided regional anesthesia. By successfully meeting these objectives, we aim to improve learner confidence and clinical ability in performing ultrasound guided nerve blocks.
The Continuous Residency Improvement Committee (CRIC) – A Novel Twist for Program Evaluation in an Academic Emergency Medicine Residency Program
DOI: https://doi.org/10.21980/J8SD17The purpose of this innovation was to develop a novel approach to continuous program evaluation and improvement using a multisource feedback design to improve resident satisfaction with the program’s responsiveness to feedback while addressing the ACGME mandate for self-study.
Realistic and Inexpensive Ultrasound Guided Paracentesis Simulator Using Pork Belly with Skin
DOI: https://doi.org/10.21980/J8NK9RBy the end of this instructional session learners should be able to: 1) Discuss the indications, contraindications, and complications associated with abdominal paracentesis; and 2) competently perform an ultrasound-guided abdominal paracentesis on a simulator and remove fluid.
Low Cost Task Trainer for Neonatal Umbilical Catheterization
DOI: https://doi.org/10.21980/J8HW6GBy the end of this instructional session learners should: 1) Discuss the indications, contraindications, and complications associated with umbilical catheterization. 2) Competently perform umbilical catheterization on the task trainer. 3) Demonstrate proper securement of the catheter.
A Low Cost Escharotomy Simulation Model for Residency Education
DOI: https://doi.org/10.21980/J8D34VBy the end of this educational session, the learner will be able to: 1) Understand the indications for an escharotomy. 2) List equipment needed to perform an escharotomy. 3) Demonstrate how to perform an escharotomy. 4) Perform an escharotomy and experience the sensation of cutting through simulated burned tissue. 5) Understand post-escharotomy management and referral to specialist.
The Use of a Social Media Based Curriculum for Newly Matched Interns Transitioning into Emergency Medicine Residency
DOI: https://doi.org/10.21980/J8F92GThis curriculum is designed to bridge this gap by fostering an environment in which incoming interns can communicate, collaborate, and practice clinical reasoning with each other and faculty prior to their arrival in residency. The goals and objectives were tailored to the Accreditation Council for Graduate Medical Education (ACGME) level 1 milestones in patient care. 1) Interpret basic ECGs; 2) Demonstrate ability to interpret basic radiographs; 3) Identify common visual diagnoses; 4) Identify common neurological emergencies on head imaging; 5) Recognize basic airway anatomy; 6) Demonstrate successful application of FOAMed resources to clinical cases; 7) Interpret common ultrasound images; 8) Describe common ED procedures; 9) Demonstrate fundamental knowledge of evidence-based medicine and biostatistics