An Unusual Case of Hematemesis
History of present illness:
A 68-year-old female presented with back pain described as burning in her mid to upper back radiating to her chest with nausea and vomiting for several hours, which progressed to active hematemesis. Her vitals were significant for hypertension (160/95) and bradycardia (57). Her exam was notable for diminished breath sounds in the bilateral bases with rhonchi in the left lung base, and epigastric tenderness without rebound or guarding. A portable X-ray followed by a computed tomography (CT) angiogram of the chest and abdomen were ordered. Upon return from CT, the patient developed hypotension, worsening bradycardia, and altered mentation.
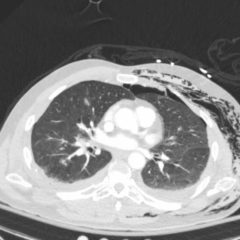
Significant findings:
The patient’schest X-ray revealed a prominent mediastinum and opacification in the left middle and lower lung fields. The CT showed an aortic aneurysm extending from the thorax to the abdomen with rupture near T7 (blue arrow). It also showed periaortic hemorrhage with active extravasation (green arrow) likely secondary to a penetrating ulcer and bilateral pulmonary opacities concerning for hemothorax (pink arrow).
Discussion:
Thoracic aortic aneurysm (TAA) is a progressive and potentially deadly disease with a poor prognosis when left untreated.1 Most TAAs are asymptomatic and may be detected incidentally on imaging. Although presentation can vary, chest or back pain might be the first presenting symptom and can represent rapid expansion, acute dissection, or rupture.2 In the acute setting, chest X-ray might be the first imaging study performed during the initial evaluation of a patient with symptoms that suggest a potential for aortic disease. Predictive sensitivity of a widened mediastinum or abnormal aortic contour can be around 64% and 71% respectively, but the sensitivity of CXR is not adequate to definitively rule out acute aortic disease.3 CT with contrast remains the imaging study of choice for diagnosis of acute thoracic aortic disease; it can be nearly 100% sensitive and can also demonstrate the presence of a dissection flap or rupture.3
Overall mortality for ruptured TAA is 97%-100%.4 While mortality is also high for repair of symptomatic TAA, repair is recommended for all symptomatic TAA (ruptured, associated with dissection, or causing pain).2 However, surgery may not be indicated based on patient comorbidities, or clinical picture. Preemptive repair of asymptomatic TAA can eliminate the risk of rupture, which is primarily predicted by size.5 Overall mortality for elective repair is 4.5% (4.6% for open repair and 3.6% for endovascular repair).6 Current guidelines suggest surgical intervention when the risk of rupture-related complications exceed the risk of surgery-related complications, which is generally around a size of 5.5 cm. However, it is also dependent on the presence of genetic risk factors for dissection and rupture, exact location, and rate of aneurysm expansion.3
In this case, cardiothoracic surgery determined that surgery would not confer any increased chance of survival based on the patient’s clinical condition, the size and location of the rupture, and the growing periaortic hemorrhage. The family decided to provide comfort measures only and the patient expired approximately one hour after presentation to the emergency department.
Topics:
Aortic aneurysm, thoracic aortic aneurysm, acute aortic syndromes, cardiothoracic surgery.
References:
- Bashir M, Fok M, Hammoud I, Rimmer L, Shaw M, Field M, et al. A perspective on natural history and survival in nonoperated thoracic aortic aneurysm patients. Aorta. 2013;1(3):182-189. doi: 10.12945/j.aorta.2013.13-043
- Woo J, Greene C. Management of thoracic aortic aneurysm in adults. In: Collins KA, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com/contents/management-of-thoracic-aortic-aneurysm-in-adults. Updated December 12, 2017. Accessed September 6, 2018.
- Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010;121(13): e266-369. doi: 10.1161/CIR.0b013e3181d4739e
- Johansson G, Markström U, Swedenborg J. Ruptured thoracic aortic aneurysms: a study of incidence and mortality rates. J Vasc Surg.1995;21(6):985-988. doi: 10.1016/s0741-5214(95)70227-x
- Davies R, Goldstein L, Coady M, Tittle SL, Rizzo JA, Kopf GS, et al. Yearly rupture or dissection rates for thoracic aortic aneurysms: simple prediction based on size. Ann Thorac Surg. 2002;73(1):17-28. doi: 10.1016/s0003-4975(01)03236-2
- Hughes K, Guerrier J, Obirieze A, Ngwang D, Rose D, Tran D, et al. Open versus endovascular repair of thoracic aortic aneurysms. Vasc Endovascular Surg.2014;48(5-6):383-387. doi: 10.1177/1538574414540484