Visual EM
Electronic Cigarette or Vaping-Associated Lung Injury Case Report
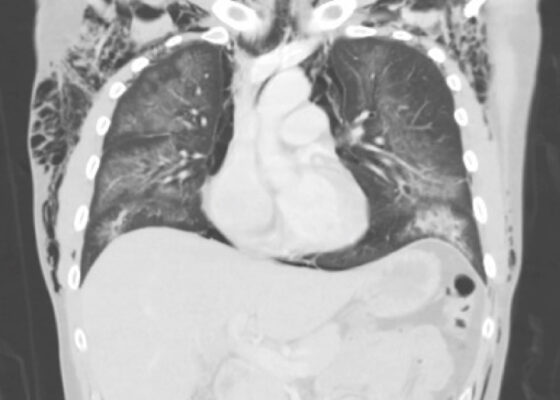
DOI: https://doi.org/10.21980/J8S65PThe CT of the chest with contrast showed subcutaneous emphysema (green star), pneumomediastinum (yellow arrow), and pneumopericardium (purple asterix) without an identifiable tracheal tear. Extensive air was visualized as hypodense areas within the chest wall within the soft tissue. The image also detailed a hypodense area surrounding the heart consistent with pneumopericardium. No disruption of the trachea was present. Additionally, the CT of the chest also showed bilateral ground glass airspace opacities (red stars) with subpleural sparing that is consistent with EVALI findings.2,5 These specific findings have been seen in many of the EVALI cases.5 This image is interesting because there is extensive pneumomediastinum with no clearly identifiable cause. The imaging shows no esophageal or tracheal or lung injury, so it is important to note relevant information collected during interview regarding patient’s recent history of vaping THC, especially when establishing a differential diagnosis.
Case Report of a Tongue-Type Calcaneal Fracture
DOI: https://doi.org/10.21980/J8NH11Examination of the right ankle demonstrated a large deformity of the superior talus with bruising and blanching of the overlying skin in the area of the Achilles tendon (see images 2,3). The remaining bones of the foot were not tender to palpation and the foot was neurovascularly intact throughout with only mild numbness in the area of the tented skin. Completing the trauma exam, the patient had no signs of head injury and no midline spinal tenderness to palpation. Inspection of the remaining long bones and joints showed no other injuries. There were mild skin scrapes on the right flank from the fall. X-rays of the right foot and ankle showed a longitudinal fracture of the calcaneal tuberosity from the articular surface to the posterior surface (see red outline) with extension into the subtalar joint (blue lines) and roughly 1.8 cm displacement between the fracture segments (yellow double arrow). These findings represented a tongue-type calcaneal bone fracture.
Mushroom for Improvement Case Report: The Importance of Involving Mycologists
DOI: https://doi.org/10.21980/J8ZW7WThe mushroom displayed here is large and lacks any gills. Small puffball mushrooms can resemble young immature button top Amanita type mushrooms. Opening the Amanita mushroom should reveal apparent gills and quickly differentiate the two- -the puffball mushroom should have a white interior without gills.
A Case Report of a Man with Burning Arm and Leg Weakness
DOI: https://doi.org/10.21980/J8V659A non-contrast computed tomography (CT) of the head and neck was performed, followed by an MRI of the cervical spine. The CT demonstrated congenital narrowing of the cervical spinal canal, with posterior disc osteophyte complex and disc bulge at C3-4 and C4-5 (arrow). The T2-weighted MRI additionally demonstrated obliteration of the anterior and posterior subarachnoid space at the level of C3-C5, with associated patchy central cord signal abnormality (arrow).
Thigh Mass Case Report
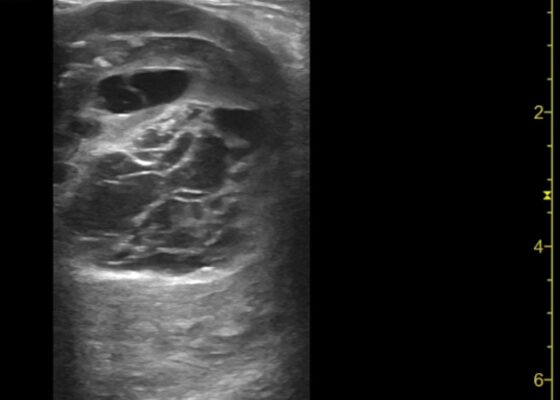
DOI: https://doi.org/10.21980/J8QD3CPoint-of-care ultrasound (POCUS) demonstrates a large, subcutaneous mass with areas of mixed echogenicity. The mass contains fluid-filled, anechoic areas with internal septations and absent doppler flow. The majority of the mass appears isoechoic to the surrounding tissues with a hyperechoic border. Computed tomography (CT) of his right thigh shows a 16 x 8.1 x 9.5 cm heterogenous, complex mass within his hamstring muscles, inferior to the femur. His lab work was significant for a white blood cell (WBC) of 17.3 (103/µL).
Inferior STEMI Electrocardiogram in a Young Postpartum Female with Sickle Cell Trait with Chest Pain – A Case Report
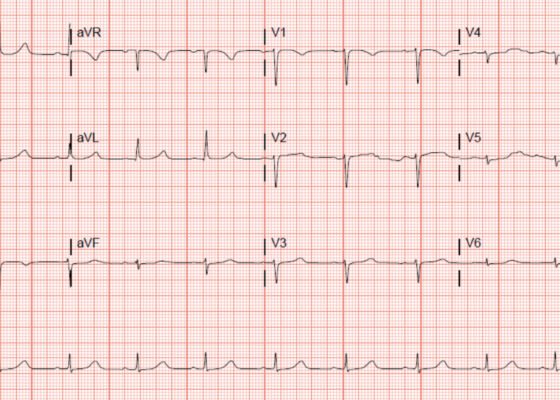
DOI: https://doi.org/10.21980/J8KP95ECG shows evidence of ST segment elevation in the inferolateral leads with reciprocal change in a bigeminy pattern. The ECG pattern seen in this patient demonstrates ST elevations in the inferior leads (II, III, and avF) as well as the precordial leads V4-V6. Reciprocal changes can also be seen in leads I and avL. Though this STEMI pattern is typically associated with occlusion of the right coronary artery in 80% of cases, it may also be caused by occlusion of the left circumflex artery. This may explain this patient’s cardiac catheterization findings of vasospasm in the left circumflex coronary artery.
Transverse Myelitis in Naloxone Reversible Acute Respiratory Failure—A Case Report
DOI: https://doi.org/10.21980/J8B659Magnetic resonance imaging of the brain, cervical, thoracic and lumbar spine without contrast was obtained and revealed increased signal throughout the spinal cord from C-1 to the conus medullaris with mild expansion consistent with transverse myelitis.
‘Cath’ It Before It’s Too Late: A Case Report of ECG Abnormalities Indicative of Acute Pathology Requiring Immediate Catheterization
DOI: https://doi.org/10.21980/J8HW7VA 12 lead ECG performed at the time of emergency department (ED) admission revealed regular sinus rhythm with noted T-wave inversion (blue arrows on Figure 1) in Lead aVL new when compared to an ECG performed a few months prior (see Figure 3). Two days later a second ECG was done when the patient developed acute chest pain while in the ICU (Figure 2) that showed persistent inversion in Lead aVL (blue arrows) as well as new J point deviation (JPD) in Leads II, aVF, V5 and V6; and new JPD in Leads V1 and V2 (green arrows) from her previous ECG while in the emergency department. These focal repolarization abnormalities did not qualify as an ST-elevation myocardial infarction by current guidelines.