Acute, massive pulmonary embolism with right heart strain and hypoxia requiring emergent tissue plasminogen activator (TPA) infusion
History of present illness:
A 63-year-old male presented to the emergency department with shortness of breath. He had a history of prostate cancer and two previous pulmonary embolisms, but was not currently on blood thinners. He had no associated chest pain at the time of presentation, but endorsed hemoptysis. Vital signs were significant for a heart rate of 88, blood pressure 145/89, oxygen saturation in the mid-70’s on room air which increased to mid-80’s on 15L facemask. His exam was significant for clear lung sounds bilaterally. He immediately underwent chest x-ray which showed no acute abnormalities. A bedside ultrasound was performed which showed evidence of right ventricular and atrial dilation, consistent with right heart strain. Given that the patient’s oxygen saturations improved to 88% on 15L facemask, the patient was felt to be stable enough for CT angiography.
Significant findings:
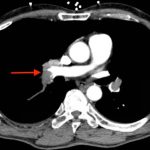
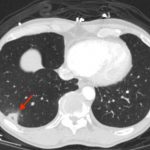
CT angiogram showed multiple large acute pulmonary emboli, most significantly in the distal right main pulmonary artery (image 1 and 2). Additional pulmonary emboli were noted in the bilateral lobar, segmental, and subsegmental levels of all lobes. There was a peripheral, wedge-shaped consolidation surrounded by groundglass changes in the posterolateral basal right lower lobe that was consistent with a small lung infarction (image 3).
Discussion:
The patient underwent in the Emergency Department a tissue plasminogen activator (TPA) infusion of alteplase 100 mg over 2 hours for his massive acute pulmonary embolisms. Throughout his TPA infusion his oxygen saturations became improved to mid-90’s and his shortness of breath symptoms began improving. His troponin returned at 0.15 ng/mL, suggesting right heart strain. He was admitted to the ICU for continued monitoring and treatment.
An acute, massive pulmonary embolism is described as having more than 50% occlusion of pulmonary blood flow.1 The main causes of hypoxia includes ventilation-perfusion mismatching and shunting.1 The indications for TPA include persistent shock or respiratory failure, evidence of moderate to severe right heart strain, and the absence of absolute contraindications to fibrinolytics.2 The dose of alteplase in acute pulmonary embolism is 100 mg over a 2-hour infusion.2
Topics:
Pulmonary embolism, ultrasound, right heart strain, TPA, CT angiography, lung infarction.
References:
- Riedel M. Acute pulmonary embolism: pathophysiology, clinical presentation and diagnosis. 2001; 85:229–240. doi: 10.1136/heart.85.2.229
- Jaff M, McMurtry M, Archer S, Cushman M, Goldenberg N, Goldhaber SZ, et al. Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolic pulmonary hypertension. Circulation, 2011;123:1788-1830.doi: 10.1161/CIR.0b013e318214914f