Posterior Reversible Encephalopathy Syndrome and Eclampsia
ABSTRACT:
Audience:
Emergency medicine residents, fellows, and recent graduates. Emergency medicine-bound senior medical students.
Introduction:
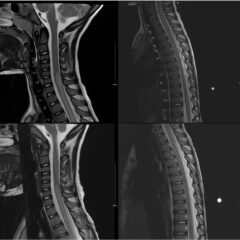
Posterior reversible encephalopathy syndrome (PRES) is an illness in which a person can present with acutely altered mentation, drowsiness or sometimes stupor, visual impairment, seizures (focal or general tonic-clonic), and sudden or constant, non-localized headaches.1 Patients at risk for developing PRES include those with underlying hypertension, preeclampsia, kidney disease, liver disease, exposure to cytotoxic medications or immunosuppressants, autoimmune disorders or sepsis. As a syndrome, PRES has gone underdiagnosed given its broad symptomatology. While it appears to affect people of all ages, it is more commonly found in middle-aged females. The underlying cause for PRES remains unclear, but some proposed mechanisms center on the dysregulation of cerebral autoregulation, the brain’s ability to maintain constant cerebral blood flow over a range of blood pressures via the constriction or dilation of the cerebral blood vessels.2 The treatment for PRES includes management of hypertension as well as diagnosing and treating the underlying etiology. This disease process needs to be recognized early by the emergency provider to reduce mortality.
Eclampsia and other hypertensive disorders in women affect as many as 10% of all pregnancies worldwide and are responsible for approximately 10% of all maternal deaths in the United States.3 Eclampsia is defined as new onset seizures in a woman with a history of preeclampsia who is between 20 weeks gestation and within four weeks postpartum.4 As an emergency medicine provider, it is imperative to be able to manage and treat a patient with eclampsia to decrease mortality and morbidity of the mother and fetus. Management of eclampsia includes treatment for seizures using magnesium sulfate, treatment for hypertension, and emergent obstetrics consult for possible delivery of the fetus.4
Educational Objectives:
At the end of this oral boards session, examinees will be able to: 1) demonstrate familiarity with the structured interview oral board format and case play; 2) recognize the history and exam features concerning for PRES and eclampsia; 3) order appropriate diagnostic workup for postpartum and hypertensive emergencies including eclampsia and PRES; 4) understand treatment options for the management of eclampsia (intravenous [IV] magnesium sulfate, IV antihypertensive therapy, and emergent consultation with an obstetrician [OB/GYN]); 5) understand threshold for taking control of airway in patients with eclampsia; 6) understand indications for ordering brain imaging in patients with eclampsia and altered mental status; and 7) demonstrate effective communication with treatment team/family members as well as correct disposition of the patient to a higher level of care (intensive care unit [ICU]).
Educational Methods:
An oral board exam-style structured interview (SI) case format was used. This allowed the learner to delve into the case in a methodical way while laying out their thought processes to better assess their medical knowledge. The case was administered as part of a multi-institution virtual Mock Oral Boards Day. Case material and instructions were distributed a week ahead of time to faculty examiners for preparation.
Research Methods:
Both learners and instructors provided written feedback after case administration. Participants gave feedback on the overall difficulty and quality of the case and provided narrative feedback on the case materials. Participants also rated the perceived effectiveness level for assessing examinees on the eight stages of patient interaction.
Results:
Of 49 examinees and six faculty examiners, 42 and four gave feedback on the case, respectively, for an overall 84% response rate. On a Likert scale from 1 (least effective) to 5 (most effective), learners rated the case at a mean 3.9 and faculty rated the case at a mean 4.3 across the eight structured stages of patient interaction. Case difficulty was rated intermediate/advanced overall. On a Likert scale from 1 (lowest quality) to 5 (highest quality), learners gave a mean rating of 3.9 and faculty gave a mean rating of 4.0. Narrative comments recommended better clarifying the history, adding a point-of-care glucose to the workup, and allowing varied magnesium sulfate dosages within the recommended range for eclampsia, and these recommendations were used to improve the case. Outside of medical knowledge aspects of this feedback, there were also comments about the structured interview format being confusing in general.
Discussion:
The educational content was found to be effective, high-quality, and intermediate-to-advanced in difficulty by both learners and faculty. From this implementation, we discovered that learners need more instruction on magnesium dosing in severe eclampsia, and also on the likelihood of concurrent PRES. Outside of the main medical knowledge take-away lessons, we have also gained insight about lack of familiarity with the structured interview format on the part of both examinees (learners) and examiners (faculty).
Topics:
Posterior reversible encephalopathy syndrome, eclampsia, preeclampsia, seizures, end-organ damage, hypertensive emergency, altered mental status, neurologic emergency, obstetric emergency, peripartum emergency, postpartum emergency.