Point-of-Care Ultrasound for the Diagnosis of Systolic Heart Failure
History of present illness:
A 52-year-old female with a history of hypertension, diabetes, and years of intravenous drug use presented to the emergency department complaining of chest discomfort and severe shortness of breath. On exam, she was tachycardic, tachypneic, and hypoxemic with rales throughout her bilateral lung fields and diffuse extremity edema. The patient’s labs were significant for a brain natriuretic peptide (BNP) of 2350.
Significant findings:
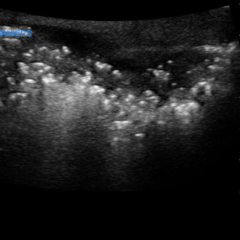
Bedside ultrasound with the phased array probe was used to obtain a parasternal long axis view which demonstrated poor contractility and a severely decreased ejection fraction (EF). M-mode was placed over the anterior leaflet of the mitral valve to create a tracing depicting both the E-wave of early diastole (green arrow) and the A-wave from the atrial kick (blue arrow). The shortest distance between the septum and the mitral valve on the M-mode tracing gives the patient’s E-Point Septal Separation (EPSS) (pink arrow). EF can be estimated using the formula EF=75.5-2.5 x EPSS (in mm). This patient’s EPSS was measured to be 20mm which estimates that she had an EF of 25.5%.
Discussion:
Ejection fracture (EF) determines how well the heart is pumping blood. It is the percentage of blood being pumped out from the left ventricle, with a normal percentage between 50%-70%. Quantifying a low EF helps in determining the severity of the systolic heart failure and assists in providing the most appropriate treatment.
Rapid assessment of EF in the emergency department is critical because patients with heart failure with preserved EF (HFpEF) clinically appear similar to patients with heart failure with reduced ejection fraction (HFrEF). Clinical trials have demonstrated that while therapies such as beta blockers, angiotensin converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs) are effective in HFrEF, these therapies do not decrease morbidity or mortality in HFpEF, suggesting that there are fundamental differences in their underlying pathophysiology. EF can be estimated using the patient’s E-point septal separation (EPSS) measured on bedside ultrasound.1 EPSS quantifies the separation between the mitral valve leaflet and the septum in early diastole.1 Measurements greater than 7mm predict depressed left ventricular function.2 The sensitivity and specificity of an EPSS measurement of greater than 7 mm for severe systolic dysfunction (left ventricular EF ≤ 30%) were 100.0% (95% confidence interval, 62.9-100.0) and 51.6% (95% confidence interval, 38.6-64.5), respectively.1 Though there is no gold standard for measuring EF,3 the most common modality is the complete echocardiogram which has a sensitivity of 80%, specificity of 88% and positive predictive accuracy of 86%.4 Bedside ultrasound allows physicians to quickly and accurately estimate a patient’s EF using EPSS in order to provide appropriate care in a timely manner.
In this case, the patient was given furosemide and nitroglycerin and admitted to the cardiac care unit. A formal cardiology echocardiogram was performed the following day that reported the patient’s EF to be 22%-30%.
Topics:
Cardiology, cardiac, ultrasound, systolic heart failure, ejection fraction, E-wave, A-wave, E-Point Septal Separation, EPSS.
References:
- McKaingney J, Krantz M, Rocque C, Hurst ND, Buchanan M, Kendall J. E-point septal separation: a bedside tool for emergency physician assessment of left ventricular ejection fraction. Am J Emerg Med. 2014;32(6):493-497. doi: 10.1016/j.ajem.2014.01.045
- Massie B, Schiller N, Ratshin R, Parmley W. Mitral-septal separation: new echocardiographic index of left ventricular function. Am J Cardiol. 1977;39(7): 1008-1016. doi: 10.1016/S00002-9149(77)80215-4
- Foley T, Mankad S, Anavekar N, et al. Measuring left ventricular ejection fraction – techniques and potential pitfalls. Eur Cardiol Rev. 2012;8(2):108-114. doi: 10.15420/ecr.2012.8.2.108
- Lehmann K, Johnson A, Goldberger A. Mitral valve E point-septal separation as an index of left ventricular function with valvular heart disease. Chest. 1983;83(1):102-108. doi: 10.1378/chest.83.1.102