Extensive Aortic Dissection with Normal Vital Signs
History of present illness:
A 63-year-old woman presented to the emergency department with one hour of chest pain, shortness of breath, jaw pain, nausea and diaphoresis. The symptoms occurred suddenly, and progressed to left arm numbness and tingling and vomiting. Her abdomen then began to hurt with radiation to her back. She was given aspirin and nitroglycerin, which did not improve her symptoms. Her blood pressure on arrival was 130/58 mmHg with a pulse of 60 beats per minute. Her clinical examination showed a 30-mmHg difference between systolic pressures in her upper extremities, decreased pulse in the left upper extremity, distant heart sounds, generalized abdominal tenderness and decreased sensation and temperature in her left arm. An electrocardiogram (ECG) showed nonspecific ST changes.
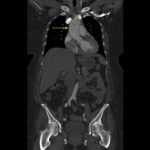
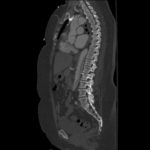
Because aortic dissection was suspected, the patient underwent urgent computed tomography (CT) angiogram of her chest, abdomen and pelvis that revealed her diagnosis.
Significant findings:
The patient was found to have a Stanford type A dissection (see yellow arrow) with visible false lumen starting at aortic arch (see green circle). The dissection extended into the descending aorta (see blue circle) as shown by the false lumen (red highlighted area) visible on CT. The radiologist performed a reconstruction of the aorta, which showed that the left kidney was not being perfused, making the kidney not visible on the reconstruction.
Discussion:
Aortic dissection is a relatively rare and life-threatening disease process. This case is unique in that she had normal vital signs despite her large aortic dissection. One must be aware of the presenting signs and symptoms in order to make a timely diagnosis. The most common presenting symptom is pain, and it is often accompanied with a new neurologic or pulse deficit. Many of the presenting symptoms are due to the location of the dissection. Stanford type A dissection refers to those proximal to the aortic arch and Stanford type B dissection refers to those distal to the aortic arch. In up to 31% percent of type A dissections, the dissection extends into the ascending arch causing a pericardial effusion, which may present with muffled heart sounds, jugular venous distension, and hypotension.1 Type A dissections may also continue into the coronary arteries, classically the right coronary artery, leading to an ST elevation myocardial infarction with the possibility of an accompanying heart block. Despite current clinical awareness, the mortality of patients with acute aortic dissection is as high as 30%.2
Contrast CT angiography (CTA) is the imaging modality of choice in stable patients, whereas transesophageal echocardiography (TEE) can be useful for a more prompt bedside diagnosis in unstable patients.3 The sensitivity and specificity of CTA is >95%.4 Stanford Type A dissection requires surgical management and Stanford type B may be managed either surgically or medically.5 In patients with type B aortic dissection, 70% present with hypertension, whereas in type A aortic dissection, 25% present with hypotension.6 Early surgical interventions can lead to decreased mortality. Studies have demonstrated a 91% survival rate after surgical repair of a type A dissection.2
In this case, the patient improved, but repeat imaging revealed 50% of her left kidney was no longer functional. However, the patient remained in stable condition and had no residual neurological deficits.
Topics:
Aortic dissection, computed tomography, chest pain.
References:
- Tsukube T, Okita Y. Cardiac tamponade due to aortic dissection: clinical picture and treatment with focus on pericardiocentesis. E-Journal of Cardiology Practice. 2017;15(18).
- Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE. Management of acute aortic dissections. Ann Thorac Surg. 1970;10(3):237–247.doi: 10.1016/S0003-4975(10)65594-4.
- von Kodolitsch Y, Schwartz, G, Nienaber C. Clinical prediction of acute aortic dissection. Arch Intern Med. 2000;160(19):2977–2982.doi: 10.1001/archinte.160.19.2977.
- Small JH, Dixon AK, Coulden RA, Flower CDR, Housden BA. Fast CT for aortic dissection. Br J Radiol. 1996; 69:900-905.
- Tsai TT. Acute Aortic Syndromes. Circulation. 2005;112(24):3802-3813. doi: 10.1161/CIRCULATIONAHA.105.534198.
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897-903. doi:10.1001/jama.283.7.897.