Ruptured AAA Presenting with Unresponsiveness and Cardiac Arrest
History of present illness:
A 75-year-old man with unknown medical history presented to the emergency department (ED) with altered mental status after being found unresponsive in the driver seat of a vehicle on the side of the road. He was hypotensive to 80/42mmHg, pale, and diaphoretic on arrival to the ED. In the ED, the patient became pulseless and was found to be in pulseless electrical activity (PEA) arrest. Cardiopulmonary resuscitation was initiated with return of spontaneous circulation achieved after four minutes. Bedside ultrasound demonstrated a 6.5-centimeter intra-abdominal mass with no appreciated free fluid or pericardial effusion. Computed tomography angiography (CTA) of the chest, abdomen, and pelvis was obtained in conjunction with emergent subspecialist consultation.
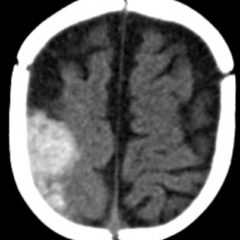
Significant findings:
Axial CT images from the CT chest, abdomen and pelvis revealed a large infra-renal abdominal aortic aneurysm measuring 7.3 x 8.2 x 10 cm with extensive mural thrombus (single white arrow) that has ruptured, with active extravasation (black arrow) of contrast into the aneurysm sac and retroperitoneum with large right retroperitoneal hematoma (multiple white arrows).
Discussion:
Abdominal aortic aneurysm (AAA) is a degenerative vascular disorder associated with sudden death due to rupture that occurs when stress on the aneurysm wall exceeds wall strength. Incidence of AAA is higher in men, in smokers, and with advancing age.1 Abdominal aortic aneurysms may be found incidentally on abdominal imaging. Unruptured aneurysms are traditionally asymptomatic.2 Symptomatic aneurysms have a variety of clinical presentations ranging from nonspecific lumbar pain to sudden cardiac arrest. Back and abdominal pain are the most common presenting symptoms, classically described as abrupt in onset and tearing in quality.3 Hypotension from blood loss can result in a shock state with evidence of end organ ischemia. Hypoperfusion of the nervous system can present as syncope.
Aneurysm diameter is the most significant predisposing factor for growth and subsequent rupture.4 Small aneurysms are defined as being less than 5.5 cm.1 Incidence of rupture in patients with AAA > 5.5 cm is estimated at 5.3% per year.5 Repeated ultrasonography, anywhere from every 6 months to every 5 years, is used to monitor the growth of an unruptured asymptomatic aneurysm once detected.6 Repair is recommended once diameter exceeds 5.5 cm because risk of spontaneous rupture exceeds risks associated with conventional open repair at this point.1
The decision to use imaging to aid in diagnosis and risk stratification varies based on clinical presentation. Patients in hypotensive shock with high clinical suspicion for ruptured AAA should have prompt surgical consultation before formal imaging studies. Bedside sonography is a non-invasive strategy that can be used during the resuscitation of an unstable patient. Sensitivity for bedside ultrasonography approaches 90% and provides useful information about size.2 Once the patient is stabilized, CTA imaging with intravenous contrast can be considered. This imaging modality can provide significantly more information about the anatomy of the aneurysm and extent of rupture but requires transport away from the resuscitation area.
Mortality in ruptured AAA can be as high as 81%. Many patients will die prior to hospital arrival and half of those presenting for medical care will die in the perioperative period.1,4,7 If cardiopulmonary resuscitation is required before surgical repair, mortality rates up to 100% have been cited.2 Management should be initiated with attempts to achieve hemodynamic stability by means of transfusion of blood products and volume expansion. A “permissive hypotension” treatment approach can be utilized where the blood pressure may be maintained in the lower than normal range in an attempt to achieve a balance between organ perfusion and hemostasis by avoiding dilutional coagulopathy and hemorrhage acceleration. Definitive management includes either immediate surgical open repair or minimally invasive endovascular aneurysm repair (EVAR). Historically, open surgical repair was the only effective treatment for AAA. However, over the last two decades, EVAR has been adopted by vascular centers as the preferred treatment due to decreased morbidity and mortality, even in unstable patients, in comparison to open repair.1,4,5 Endovascular aneurysm repair consideration requires further assessment of aneurysm morphology, typically by CT imaging, and suitability is determined based on eligibility criteria by the stent-graft manufacturer, such as assessment of the aortic neck (region immediately below the renal arteries) morphology.5
In this case, the patient was taken to the operating room for open repair by vascular surgery and died intra-operatively.
Topics:
Abdominal aortic aneurysm, ruptured abdominal aortic aneurysm, etiologies of cardiac arrest.
References:
- Badger S, Forster R, Blair PH, Ellis P, Kee F, Harkin DW. Endovascular treatment for ruptured abdominal aortic aneurysm. Cochrane Database of Syst Rev. 2017;5:CD005261.
- Sakalihasan N, Limet R, Defawe OD. Abdominal aortic aneurysm. Lancet. 2005;365(9470):1577-1589.
- Prince LA, Johnson GA. Aneurysmal disease. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM, eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 8th New York, NY: McGraw-Hill; 2016:416-419.
- Broos PP, Mannetje YW, Loos MJ, et al. A ruptured abdominal aortic aneurysm that requires preoperative cardiopulmonary resuscitation is not necessarily lethal. J Vasc Surg. 2016;63(1):49-54.
- England A, Mc Williams R. Endovascular aortic aneurysm repair (EVAR). Ulster Med J. 2013;82(1):3-10.
- Guirgius-Blake JM, Beil TL, Sun X, Senger CA, Whitlock EP. Primary care screening for abdominal aortic aneurysm: a systematic evidence review for the U.S. preventive services task force. Rockville, MD: Agency for Healthcare Research and Quality; 2014.
- Schmitz-Rixen T, Keese M, Hakimi M, et al. Ruptured abdominal aortic aneurysm – epidemiology, predisposing factors, and biology. Langenbecks Arch Surg. 2016;401(3):275-288.
- Greenhalgh RM, Brown LC, Powell JT, et al. Endovascular versus open repair of abdominal aortic aneurysm. N Engl J Med. 2010;362(20):1863-1871.