Peritonsillar Abscess Model for Ultrasound Diagnosis Using Inexpensive Materials
ABSTRACT:
Audience:
This low-cost peritonsillar abscess model is intended for the education of emergency medicine and otolaryngology residents and advanced care practitioners of all training levels.
Introduction:
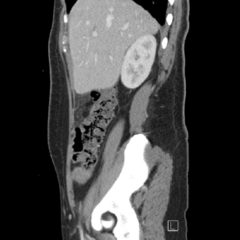
With incidence rates as high as 124 per 100,000 in the 14-21 age range, peritonsillar abscesses (PTA) are one of the more common head and neck soft tissue infections encountered in the emergency department.1 Peritonsillar abscesses can present to the emergency department in critically ill patients with the dangers of airway compromise and further local spreading. Emergency medicine (EM) residents need practice to properly identify and to minimize procedural complications such as perforation of nearby vessels, aspiration pneumonitis, and airway compromise. A major tool used in the emergency department that can help prevent complications is the use of ultrasound, which the Accreditation Council for Graduate Medical Education (ACGME) requires residents to become proficient at.2 Historically, computed tomography (CT) scanning to diagnose along with blind drainage has been the method of choice. With a sensitivity of 95.2%, intraoral ultrasound can minimize both radiation and procedure related complications.3 The current simulators available come at significant capital expenditure and do not provide high-fidelity ultrasound experience. Here we design and implement a low-cost trainer for residents to use ultrasound to diagnose and drain a PTA.
Educational Objectives:
By the end of this instructional session learners should be able to: 1) identify and discuss the indications, contraindications, and complications associated with peritonsillar abscesses, 2) properly identify and measure a PTA through ultrasound, and 3) competently perform ultrasound-guided peritonsillar abscess drainage on a simulator and remove fluid.
Educational Methods:
This PTA model utilizes task trainers designed from Styrofoam wig heads. An airway was modeled using readily available wood shop tools and balloons filled with a fluid mixture containing coconut lotion, water, and fragrance beads, which were inserted into the airway. This unique mixture within the balloons creates a realistic echogenicity of an abscess with loculations. With emergency medicine clinical faculty guidance and the use of ultrasound, learners are able to identify a peritonsillar abscess and subsequently demonstrate drainage of fluid with a needle and syringe.
Research Methods:
This PTA model was tested with a group of 36 emergency medicine residents. Optional, anonymous post surveys were completed by 17 residents. A 5-point Likert Scale was used to assess utility of this model.
Results:
The majority of users agreed the model provides a realistic image of the disease for diagnosis by ultrasound with a score of 3.6 and felt more comfortable identifying and draining peritonsillar abscesses with scores of 3.7 and 3.6 respectively. Learners’ surveys revealed the session was useful and improved their knowledge with both scoring 3.8. No critical feedback was given by learners or instructors. The efficacy of the content was assessed by evaluators observing proper ultrasound, procedure set up, and drainage of PTA.
Discussion:
This inexpensive model to expose residents to proper PTA drainage was effective considering learners’ high response to post-procedure survey scales. The results of our pilot implementation showed this model has utility in teaching ultrasound guided identification and drainage of PTA’s. With minimal build and optimized instruction time, we can improve residents’ comfort in performing this procedure and allow for important simulation experience in a safe, controlled environment.
Topics:
Simulation, emergency medicine, peritonsillar abscess, otolaryngology.