Little Patients, Big Tasks – A Pediatric Emergency Medicine Escape Room
ABSTRACT:
Audience:
The target audience for this small group session is post-graduate year (PGY) 1-4 emergency medicine (EM) residents, pediatric EM (PEM) fellows, and medical students.
Introduction:
Pediatric emergency department visits have been declining since the start of the COVID-19 pandemic, leading to decreased exposure to pediatric emergency care for EM residents and other learners in the ED.1 This is a major problem, given that the Accreditation Council for Graduate Medical Education (ACGME) mandates that a minimum of 20% of patient encounters or five months of training time for EM residents must occur with pediatric patients, with at least 50% of that time spent in the ED setting.2,3 A minimum of 12 months must be spent in the pediatric ED for PEM fellows,2 and an average of 7.1 weeks of medical school are spent in pediatric clerkships.4 This decrease in pediatrics exposure in the post-pandemic environment can be addressed through simulation and gamification. We selected the gamification method of an escape room to create an engaging environment in which learners could interface with key pediatric emergency medicine clinical concepts via group learning.
Educational Objectives:
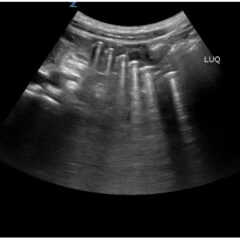
By the end of this small group exercise, learners will be able to: 1) demonstrate appropriate dosing of pediatric code and resuscitation medications; 2) recognize normal pediatric vital signs by age; 3) demonstrate appropriate use of formulas to calculate pediatric equipment sizes and insertion depths; 4) recognize classic pediatric murmurs; 5) appropriately diagnose congenital cardiac conditions; 6) recognize abnormal pediatric electrocardiograms (ECGs); 7) identify life-threatening pediatric conditions; 8) demonstrate intraosseous line (IO) insertion on a pediatric model; and 9) demonstrate appropriate use of the Neonatal Resuscitation Protocol (NRP®) algorithms.
Educational Methods:
An escape room – a form of gamification – was utilized to engage the learners in active learning. Gamification is an increasingly popular educational technique being utilized in graduate medical education and refers to the conversion of serious, non-trivial material into a fun activity fashioned like a game in order to enhance engagement in learning.5 This educational method seeks to enhance knowledge, attitudes, and skills via components of games – such as puzzles and prizes – outside of the context of a traditional game.6 Though high-quality research data on the effectiveness of gamification methods in graduate medical education is limited, studies have shown that gamification enhances learning, attitudes, and behaviors.5,7 One randomized, clinical-controlled trial investigating the use of gamification to enhance patient outcomes found that patients of primary care physicians randomized to the gamification group reached blood pressure targets faster than in the control group.8 Escape rooms as a modality for education have been suggested to improve active learning and enhance learner engagement in the learning process.9 In an escape room, learners are “locked” in an artificial environment (whether digitally or in person) and must utilize their group or individual knowledge to solve puzzles and escape from their “entrapment.”9,10 Escape rooms utilized as part of EM residency didactic training have demonstrated learner enthusiasm,11,12 desire to repeat the activity again,13 preference for escape rooms over traditional learning methods,14,15 improved confidence in communication and leadership skills,11,15 and improvement scores from pre- to post-testing.16
We developed an escape room in which learners were divided into teams and informed that they would need to “escape” from our resident lounge by successfully completing all nine stations. The first team to complete all nine stations would win a prize. Only after the last team completed the ninth station and debriefing was complete could all teams be “freed” from the escape room.
Research Methods:
Learners provided anonymous online survey feedback regarding the quality of the educational content and the efficacy of the delivery method.
Results:
A post-participation survey was disseminated to 55 residents, 32 of whom attended the PEM Escape Room, with a response rate of 9% (3/32 residents). One hundred percent of respondents felt that the activity content was applicable to their needs as an emergency physician. The session was rated as excellent by 33.3% of respondents, and 66.7% of respondents rated the session as above average. A second survey was disseminated seven months after the event to the 24 remaining residents who attended the event, with a response rate of 46% (11/24 residents); eight attendees had graduated at the time of this survey dissemination. Results of the second survey indicated that 100% (24/24 residents) felt that the activity content was applicable to their needs as an emergency physician, 73% (17/24 residents) rated the session as excellent, and 27% (7/24 residents) rated the session as above average.
Discussion:
Though we received limited survey responses (3/32 on the first survey and 11/24 on the second survey), respondents felt that the educational content met their learning needs and was of high quality. We had six faculty members present to facilitate the escape room while there were four groups of residents (eight per group). The ideal faculty to resident ratio would be one faculty member per group with three to six players, based on prior literature showing that teams of more than six players take longer to complete escape room tasks.17,18 We also recognized the importance of sending out the feedback survey link early because we believe the delay in our survey being emailed to the residents contributed to the low response rate (three trainees).
One participant provided the following feedback: “I think the ‘escape room’ struck an excellent balance with regard to trying to address knowledge that was relevant but also obscure or difficult enough that group/collaborative effort was required. I enjoyed the process and low stakes atmosphere.” This quote nicely summarizes our take-aways: That the PEM escape room incorporates key tenets of adult learning theory. Also known as andragogy, adult learning theory posits that adult learners are self-directed, have prior life experiences that shape their learning process, learn for practical reasons (ie, choose to learn in order to fulfill the demands of their social role), and are problem-oriented in their learning.19 Though andragogy does not technically apply only to adults (as many children are self-directed learners),20 having an understanding of the practical and experiential nature via which adults approach learning allows the adult educator to appropriately cater educational activities to meet the adult learner’s needs.
This escape room aligned with the core tenets of adult learning theory in several ways. Specifically, residents were given autonomy of participation in the escape room and thus had to take initiative to promote their own learning.21 Topics featured in the escape room stations were selected based on their clinical challenges and high-yield for board examinations and patient care, making their relevance immediately obvious to learners; this is a key feature of catering to adult learners.22 The escape room provided a comfortable and collegial environment in which residents felt comfortable learning, fostering an ideal setting for mature learners.21 Direct and immediate feedback are key components of adult learning theory, and faculty members were physically present to provide feedback at each escape room station.22 Finally, working in teams required the learners to engage in active learning rather than acting as passive recipients of cognitive information.21 Thus, the PEM escape room serves as an ideal framework to meet the needs of the adult learner.
Topics:
Pediatrics, emergency medicine, pediatric emergency medicine.