Neurology
Guillain-Barrè
DOI: https://doi.org/10.21980/J8TH06At the conclusion of the simulation session, learners will be able to: 1) Recognize the clinical signs and symptoms associated with Guillain-Barré syndrome, including muscle weakness and hyporeflexia. 2) Identify abnormal vital signs secondary to dysautonomia. 3) Discuss evaluation for impending respiratory failure, including bedside pulmonary function testing. 4) Discuss the management of Guillain-Barré, including management of dysautonomia and respiratory failure, as well as definitive management with plasmapheresis versus intravenous immunoglobulin. 5) Appropriately disposition the patient to the intensive care unit. 6) Effectively communicate with team members and nursing staff during resuscitation of a critically ill patient
Radial Nerve Palsy
DOI: https://doi.org/10.21980/J8KS7FOn physical exam, the patient was unable to extend his right wrist, thumb, and fingers, and had no sensation of his 1stdorsal interosseous muscles up to the proximal dorsal radial aspect of his forearm. The patient also had slight weakness in thumb abduction. Triceps strength was preserved.
Viridans streptococci Intracranial Abscess Masquerading as Metastatic Disease
DOI: https://doi.org/10.21980/J8CH05A non-contrast CT (Figure 1) revealed a large hypoattenuating left parietal lesion. When the CT was enhanced with intravenous contrast (Figure 2), the same lesion showed peripheral rim enhancement, suggestive of a brain abscess.
Dense MCA Sign
DOI: https://doi.org/10.21980/J8CS66A non-contrast computed tomography (CT) scan showed a hyperdensity along the right middle cerebral artery (MCA) consistent with acute thrombus. The red arrow highlights the hyperdensity in the annotated image.
Status Epilepticus in the Emergency Department
DOI: https://doi.org/10.21980/J8RC7VAt the end of this simulation session, the learner will: 1) Demonstrate the management of status epilepticus 2) Justify when airway intervention is needed for status epilepticus 3) Describe risk factors for status epilepticus 4) Prepare a differential diagnosis for the causes in status epilepticus.
Presentation of Significant Subarachnoid Hemorrhage without Loss of Consciousness
DOI: https://doi.org/10.21980/J80W29A non-contrast head CT demonstrated extensive subarachnoid hemorrhage occupying both cerebral convexities, the anterior interhemispheric fissure, the sylvian fissures, and the basal cisterns. Later CTA would show an 8 mm by 7 mm by 8mm MCA aneurysm near the M1/M2 junction and two pericallosal artery aneurysms, 7 by 6 mm and 8 by 5 mm respectively.
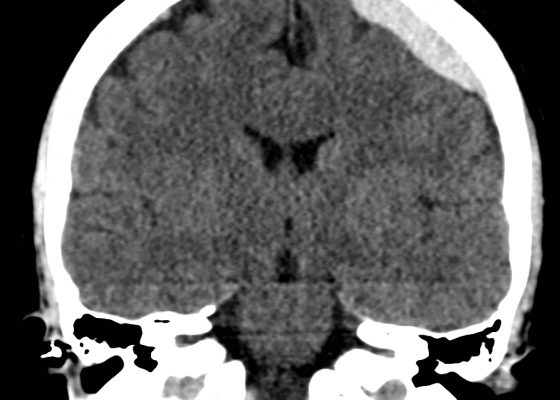
Acute Subdural Hematoma
DOI: https://doi.org/10.21980/J87C76Non-contrast Computed Tomography (CT) of the Head showed a dense extra-axial collection along the left frontal and parietal regions, extending superior to the vertex with mild mass effect, but no midline shift.