Cardiology/Vascular
Asymptomatic Wolff-Parkinson-White Syndrome: Incidental EKG
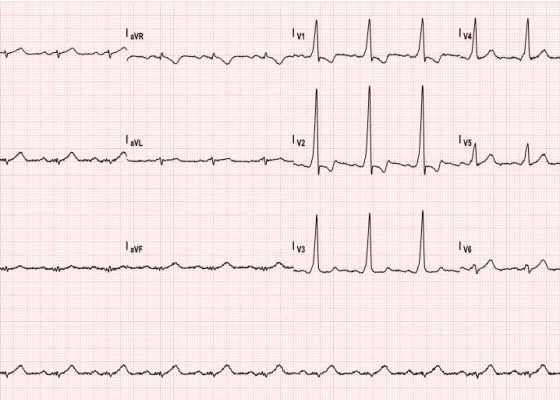
DOI: https://doi.org/10.21980/J8T05XThe ECG shows slurred up-stroking of the QRS complexes characteristic of a delta wave. The PR interval is normal; however, the QT interval is greater than 110ms.
Renal Infarction from Type B Aortic Dissection
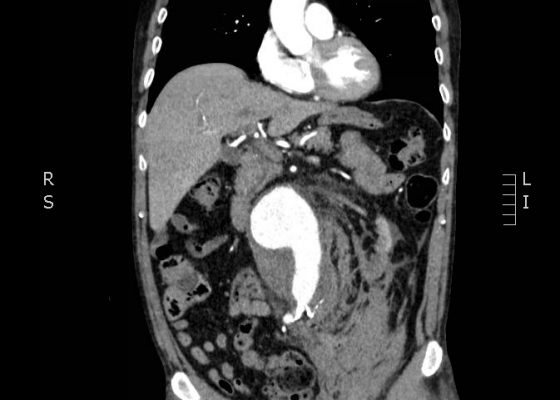
DOI: https://doi.org/10.21980/J8HG9GInitial abdominal images demonstrated a dissection flap; therefore, a CTA of the chest was also obtained. These images revealed a Stanford type B aortic dissection beginning just distal to the left subclavian artery and extending to the origin of the inferior mesenteric artery. The right renal artery arose from the true lumen of the dissection while the left renal artery arose from the false lumen. This case is interesting as imaging shows the lack of perfusion to the left kidney, residing in the retroperitoneum, which correlates with her non-descript abdominal and left flank pain.
Ruptured Abdominal Aortic Aneurysm
DOI: https://doi.org/10.21980/J8FP6SCTA demonstrated a ruptured 7.4 cm infrarenal abdominal aortic aneurysm with a large left retroperitoneal hematoma.
Use of Bedside Compression Ultrasonography for Diagnosis of Deep Venous Thrombosis
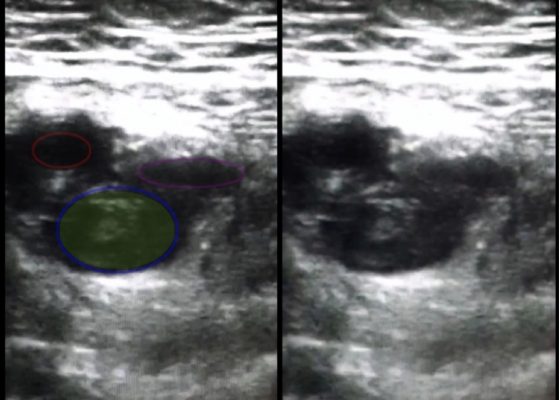
DOI: https://doi.org/10.21980/J81G94As shown in the still image of the performed ultrasound, a transverse view of the proximal-thigh revealed a visible thrombus (green shading) occluding the lumen of the left common femoral vein (blue ring), which was non-compressible when direct pressure was applied to the probe. Also visible is a patent and compressible branch of the common femoral vein (purple ring) and the femoral artery (red ring), highlighted by its thick vessel wall and pulsatile motion.
Emed-Opoly: Echocardiography
DOI: https://doi.org/10.21980/J8PC77By the end of this session, the learner will be able to:
1) Recognize normal and abnormal left heart global function
2) Recognize normal and abnormal right heart global function
3) Recognize pericardial effusions and pericardial tamponade
Left Ventricular Assist Devices
DOI: https://doi.org/10.21980/J8JP4ZUpon completion of this cTBL module, the learner will be able to: 1) Properly assess LVAD patients’ circulatory status; 2) appropriately resuscitate LVAD patients; 3) identify common LVAD complications; 4) evaluate and appropriately manage patients with LVAD malfunctions.
Acute Aortic Dissection Presenting Exclusively as Lower Extremity Paresthesias
DOI: https://doi.org/10.21980/J8NK57Chest x-ray and CT angiogram was performed to evaluate his thoracic and abdominal vasculature. Chest x-ray did not show any significant widening of the mediastinum. The CT angiogram demonstrated an intimal tear along the aortic arch separating a true and false aortic lumen, consistent with an acute aortic dissection. The true lumen (highlighted in blue in images 1-5) can be identified by continuity with an undissected part of the aorta. While the false lumen (highlighted in red in images 1-5) can be identified by its crescent shape and larger cross-sectional area.
Acute, massive pulmonary embolism with right heart strain and hypoxia requiring emergent tissue plasminogen activator (TPA) infusion
DOI: https://doi.org/10.21980/J84K5KCT angiogram showed multiple large acute pulmonary emboli, most significantly in the distal right main pulmonary artery (image 1 and 2). Additional pulmonary emboli were noted in the bilateral lobar, segmental, and subsegmental levels of all lobes. There was a peripheral, wedge-shaped consolidation surrounded by groundglass changes in the posterolateral basal right lower lobe that was consistent with a small lung infarction (image 3).