Posts by JETem
Meningococcal Meningitis with Waterhouse-Friderichsen Syndrome
DOI: https://doi.org/10.21980/J8TH1KBy the end of this simulation session, learners will be able to: (1) manage a patient with altered mental status (AMS) with fever while maintaining a broad differential diagnosis, (2) recognize the risk factors for meningococcal meningitis, (3) manage a patient with worsening shock and perform appropriate resuscitation, (4) develop a differential diagnosis for thrombocytopenia and elevated international normalized ratio (INR) in an altered febrile hypotensive patient with rash, (5) manage the bleeding complications from WFS, (6) discuss the complications of meningococcal meningitis including WFS, and (7) review when meningitis prophylaxis is given.
Eclampsia
DOI: https://doi.org/10.21980/J8PS8RBy the end of this simulation session, learners will be able to: 1) demonstrate care of a gravid patient with altered mental status; 2) demonstrate care of a gravid patient with seizures; 3) recognize care involved in assessment of fetal status; 4) execute appropriate subspecialty consultation; 5) recognize the clinical signs and symptoms of eclampsia; 6) distinguish different treatment options for eclampsia; 7) identify magnesium toxicity and reversal agent; and 8) differentiate the spectrum of preeclampsia.
Tracheoinnominate Artery Fistula
DOI: https://doi.org/10.21980/J8K05RBy the end of this simulation, learners will be able to: 1) perform a focused history and physical exam on any patient who presents with bleeding from the tracheostomy site, 2) describe the differential diagnosis of bleeding from a tracheostomy site, including a TIAF, 3) demonstrate the stepwise management of bleeding from a suspected TIAF, including cuff hyperinflation and the Utley Maneuver, 4) verify that definitive airway control via endotracheal intubation is only feasible in the tracheostomy patient when it is clear, upon history and exam, that the patient can be intubated from above, 5) demonstrate additional critical actions in the management of a patient with a TIAF, including early consultation with otolaryngology and cardiothoracic surgery as well as emergent blood transfusion and activation of a massive transfusion protocol.
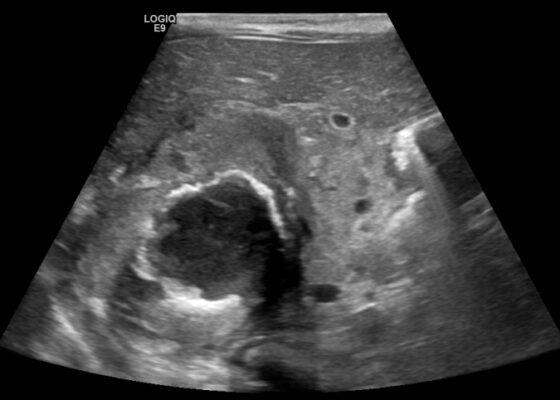
A Case Report of Glycogenic Hepatopathy
DOI: https://doi.org/10.21980/J8SQ0ZThe ultrasound images reveal hepatomegaly and an increased echogenicity of the liver parenchyma that is diffuse. The increased echogenicity can be best appreciated by a comparison to surrounding structures. It is important to note that the increased echogenicity is non-focal and consistent throughout the entire liver in multiple views. These findings can be consistent with nonalcoholic steatohepatitis as well as glycogenic hepatopathy.
A Case Report of a Large Goiter Resulting in Tracheal Deviation
DOI: https://doi.org/10.21980/J80645In the image, one can see significant tracheal deviation around the right side of the mass (black arrows). This degree of deviation would make ventilation in a paralyzed patient extremely difficult, if not impossible.
Case Report—Pediatric Brugada Phenotype from Accident Cocaine Ingestion
DOI: https://doi.org/10.21980/J8VH28Initial EKG was concerning for type I Brugada pattern with an incomplete right bundle branch block in V1 & ST segment elevation terminating in an inverted T wave in V2. There are also signs of sodium channel toxicity with a widened QRS complex, tachycardia and a terminal R wave present in aVR where the R wave is bigger than the S wave or the R wave is over 3mm in aVR.
A Case Report of Neonatal Vomiting due to Adrenal Hemorrhage, Abscess and Pseudohypoaldosteronism
DOI: https://doi.org/10.21980/J8QQ0BAn ultrasound (US) of the abdomen was obtained to evaluate for possible pyloric stenosis (see US transverse/dopper imaging). While imaging showed a normal pyloric channel, it revealed an unexpected finding: a complex cystic mass arising from the right adrenal gland (yellow outline), measuring 5.8 by 4.0 by 6.4 cm with calcifications peripherally and mass effect on the kidney without evidence of vascular flow (blue arrow). Computed tomography (CT) of the abdomen/pelvis with IV contrast was subsequently obtained and measured the lesion as 2.8 by 4.6 by 4 cm without evidence of additional masses, lymphadenopathy or left adrenal gland abnormality (see CT axial, coronal, and sagittal imaging).
Case Report of Unusual Facial Swelling in an 8-Month-Old
DOI: https://doi.org/10.21980/J8M06FFacial ultrasound revealed local inflammatory changes such as increased echogenicity and heterogeneity in the soft tissues of the right cheek, suggestive of soft tissue edema. There was evidence of a prominent right parotid gland with increased heterogeneity suggestive of a traumatic injury. Additionally, facial ultrasound demonstrated a 6mm ill-defined anechoic collection within the right cheek without increased doppler flow (green arrow), thought to represent a focal area of edema instead of an abscess.