Ophthalmology
Case Report of Herpes Zoster Ophthalmicus with Concurrent Parotitis
DOI: https://doi.org/10.21980/J8R93NThe presence of soft tissue stranding about the parotid gland suggested an underlying inflammatory or infectious process of the parotid gland. Cellulitis was considered as a possible diagnosis as well, given the presence of soft tissue stranding in the dermis that is adjacent to the parotid gland. Fortunately, no enhancement was seen in local muscles, fascia, or bones to suggest a myositis, fasciitis, or osteomyelitis. By using the anatomy of the patient and understanding the changes that occur on CT when inflammation is present, the appropriate depth and location of infection can be made, allowing for appropriate treatment regimens.
Use of An Ophthalmology Tutorial to Improve Resident Comfort with the Emergency Eye Exam
DOI: https://doi.org/10.21980/J86H0MBy the end of this small group didactic, learners will be able to: 1) demonstrate ability to focus on the various components of the slit lamp exam 2) demonstrate understanding of a systematic approach to the eye exam 3) demonstrate appropriate use of the Diaton, iCare, and Tonopen tonometers.
Vitreous Hemorrhage Case Report
DOI: https://doi.org/10.21980/J88D3BPoint of care ultrasound (POCUS) revealed hyperechoic material in the vitreous consistent with a vitreous hemorrhage. On the ultrasound images, there is visible hyperechoic debris seen floating in the vitreous as the patient moves his eye. Since the vitreous is typically anechoic (black) in color on ultrasound, turning up the gain on the ultrasound machine makes these findings easier to see and often highlights abnormalities, such as this hemorrhage (see annotated still).
Case Report of a Man with Right Eye Pain and Double Vision
DOI: https://doi.org/10.21980/J8KW7GABSTRACT: A 39-year-old previously healthy male presented with three days of right eye pressure and one day of binocular diplopia. He denied history of trauma, headache, or other neurological complaints. He had normal visual acuity, normal intraocular pressure, intact convergence, and no afferent pupillary defect. His neurologic examination was non-focal except for an inability to adduct the right eye past midline
Build Your Own Eye: A Method for Teaching Ocular Anatomy and Pathophysiology
DOI: https://doi.org/10.21980/J8GS8WBy the end of this session the participant will be able to: 1) Describe basic anatomy of the eye, 2) Build a basic model of the eye, 3) Identify which diseases are associated with which parts of the eye, 4) Identify the pathophysiology behind diseases of the eye, 5) Name correct treatment for each disease.
The Eyes Have It: A Low-Cost Model for Corneal Foreign Body Removal Training
DOI: https://doi.org/10.21980/J82S85ABSTRACT: Audience: This corneal foreign body simulator is designed to instruct junior emergency medicine (EM) residents and medical students with an interest in emergency medicine. Introduction: Eye complaints are common in the emergency department (ED), accounting for approximately 2 million ED visits each year.1 Corneal foreign bodies (CFB) account for approximately 7.5% of these presentations, and many EM providers are
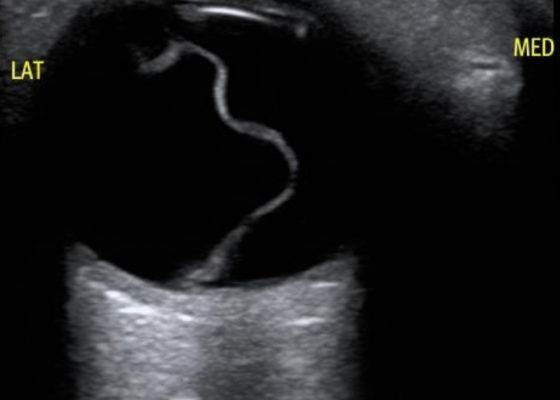
Posterior Vitreous Detachment
DOI: https://doi.org/10.21980/J89K9NOcular ultrasound was performed and demonstrated a thin, slightly echogenic strand (blue arrow) extending from the posterior eye into the vitreous humor (yellow arrow) which was hyperkinetic with extraocular motion. These findings are consistent with a posterior vitreous detachment (PVD).
Macula-Off Retinal Detachment Identified on Bedside Ultrasound
DOI: https://doi.org/10.21980/J8WP8KPoint-of-care ultrasound was performed, demonstratinga free-floating, serpiginous, hyperechoic membrane (R) tethered at the optic nerve (ON) and ora serrata (OS), but detached at the macula (M) lateral to the optic nerve. This is diagnostic for macula-off retinal detachment. It can be differentiated from macula-on retinal detachment, in which the hyperechoic retina would appear attached posteriorly at the location of the macula just lateral to the optic nerve. Ophthalmology was consulted, agreed with the diagnosis of macula-off retinal detachment, and took the patient to the OR for laser photocoagulation.