Posts by JETem
Thyroid Storm
DOI: https://doi.org/10.21980/J8XD03By the end of this simulation session, the learner will be able to: 1) understand the essential physical exam components necessary to evaluate for etiologies of acute encephalopathy, 2) review laboratory and imaging studies to obtain for evaluation of acute encephalopathy and/or suspected thyroid storm, as well as the rationale behind ordering each study, 3) identify underlying etiologies or pathologies for developing thyroid storm, 4) discuss treatment for thyroid storm.
A Simulated Scenario to Improve Communication Skills of Residents Providing Online Medical Command of Emergency Medical Service Providers
DOI: https://doi.org/10.21980/J8SK8MBy the end of this simulation, learners will be able to: 1) discuss appropriate medical command instructions for pediatric cardiac arrest; 2) describe alternative methods to obtain weight-based dosing of pediatric critical care medications, if Broselow tape is unavailable; 3) identify need for a definitive airway in a pulseless patient without interruption of chest compressions.
Identify need for rapid intraosseous access in a pulseless pediatric patient; 4) describe the indications for helicopter transfer in a critically ill child.
Post-Termination Hemorrhage
DOI: https://doi.org/10.21980/J8NW6QBy the end of this simulation, participants will be able to: 1) recognize post-termination hemorrhage and hemorrhagic shock; 2) demonstrate appropriate acute resuscitation for a patient with hemorrhagic shock; 3) review the differential diagnosis for a patient with post-termination hemorrhage; 4) identify the indications for massive transfusion protocol.
Thyroid Storm in the Emergency Department
DOI: https://doi.org/10.21980/J8234RBy the end of this simulation-based session, the learner will be able to: 1) Recognize the signs and symptoms of thyroid storm and appropriately diagnose a patient with thyroid storm. 2) Choose appropriate medications for the treatment of thyroid storm. 3) Determine the appropriate disposition for a patient presenting in thyroid storm. 4) Discuss the rationale behind each drug used to treat thyroid storm. 5) List at least three precipitants of thyroid storm.
A Story About Mesenteric Ischemia
DOI: https://doi.org/10.21980/J8J33QWe aim to teach the presentation and management of cardiovascular emergencies through the creation of a flipped classroom design. This unique, innovative curriculum utilizes resources chosen by education faculty and resident learners, study questions, real-life experiences, and small group discussions in place of traditional lectures. In doing so, a goal of the curriculum is to encourage self-directed learning, improve understanding and knowledge retention, and improve the educational experience of our residents.
Emergency Medicine Curriculum Utilizing the Flipped Classroom Method: Infectious Disease and Immunology
DOI: https://doi.org/10.21980/J8DD1TWe aim to teach the presentation and management of infectious disease and immunological emergencies through the creation of a flipped classroom design. The topics include sepsis, sexually transmitted infections (STIs), tropical diseases, angioedema and anaphylaxis, transplant-related emergencies, and collagen vascular diseases. This unique, innovative curriculum utilizes resources chosen by education faculty and resident learners, study questions, real-life experiences, and small group discussions in place of traditional lectures. The goal of our curriculum is to encourage self-directed learning, improve understanding and knowledge retention, and improve the educational experience of our residents.
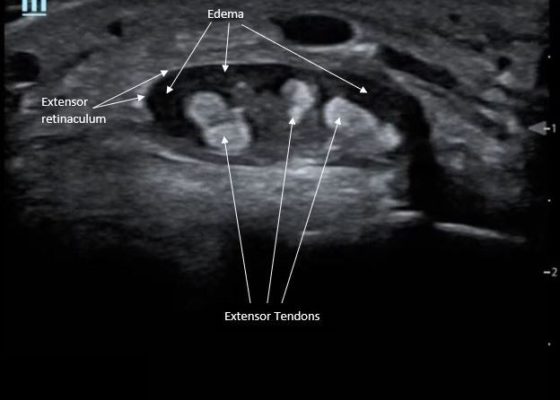
Point-Of-Care Ultrasound for the Diagnosis of Extensor Tenosynovitis
DOI: https://doi.org/10.21980/J8Q050Point-of-care ultrasound of the dorsal aspect of the left hand reveals a heterogenous hypoechoic fluid collection surrounding the extensor tendons (axial view) within the retinaculum consistent with edema. Longitudinal view shows anechoic fluid within the tenosynovium which is located between the anisotropic extensor tendon and linear hyperechoic synovial sheath. Longitudinal view also shows some cobblestoning, or tissue edema, superficial to the anisotropic extensor tendon. The patient’s contralateral right dorsal hand was scanned in a longitudinal view and shows no cobblestoning or hypoechoic fluid under the synovial sheath. The patient was diagnosed with tenosynovitis, and started on intravenous antibiotics.
Point-of-care Ultrasound in the Diagnosis and Monitoring of Bladder Hematoma vs. Hemorrhage
DOI: https://doi.org/10.21980/J8092FBladder POCUS demonstrated 500mL of post void residual fluid, indicative of retention. Half of the volume is hyperechoic (red circle); this is likely the bladder wall hematoma. Could also consider sonographic artifact, bladder mass, or cystitis.1-2