Spontaneous Pneumomediastinum: Hamman Syndrome
History of present illness:
A 28-year-old female presented to the Emergency Department (ED) with three days of intermittent, epigastric abdominal pain and non-bloody, non-bilious emesis with occasional diarrhea. She had a history of gastric cancer complicated by gastric outlet obstruction requiring gastric stent, and was receiving treatment with chemotherapy. She was originally diagnosed two months prior to this visit, after an emergent right salpingo-oophorectomy for possible ovarian torsion revealed an ovarian mass consistent with a Krukenberg tumor. Upon presentation to the ED, her only complaints were of vomiting and abdominal pain, with no additional symptoms. Based on the initial clinical presentation, abdominal and pelvic computerized tomography (CT) scans, surgical and gastrointestinal (GI) consultations, and general labs were ordered for the patient.
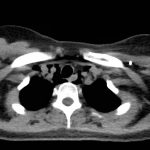
The initial CT scan found pneumomediastinum, which prompted a thoracic CT scan with contrast to determine the etiology and extent of the condition in the patient. The results of the scan prompted the treating ED physicians to consider esophageal perforation. Following consultation, the surgical and GI physicians did not recommend engaging acute intervention. Laboratory evaluation demonstrated mild hypokalemia and hyponatremia, both of which were addressed by administering intravenous (IV) fluids.
The patient was hospitalized for chemotherapy-induced nausea and received prophylactic IV piperacillin-tazobactam. She remained afebrile, hemodynamically stable with negative blood cultures, and was discharged to complete an additional seven-day course of amoxicillin-clavulanic acidwith scheduled ondansetron.
Significant findings:
The initial CT scans showed extraluminal gas surrounding the distal esophagus as it traversed the posterior mediastinum, concerning for possible distal esophageal perforation that prompted surgery and GI consultations. There was no evidence of a drainable collection or significant fat stranding. The image also showed an intraluminal stent traversing the gastric antrum and gastric pylorus with no indication of obstruction. Circumferential mural thickening of the gastric antrum and body were consistent with the patient’s history of gastric adenocarcinoma. The shotty perigastric lymph nodes with associated fat stranding, along the greater curvature of the distal gastric body suggested local regional nodal metastases and possible peritoneal carcinomatosis.
The thoracic CT scans showed extensive pneumomediastinum that tracked into the soft tissues of the neck, which given the history of vomiting also raised concern for esophageal perforation. There was still no evidence of mediastinal abscess or fat stranding. Additionally, a left subclavian vein port catheter, which terminates with tip at the cavoatrial junction of the superior vena cava can also be seen on the image.
Discussion:
Spontaneous Pneumomediastinum, also known as Hamman syndrome, is defined by the uncommon incidence of free air in the mediastinum due to the bursting of alveoli, as a result of extended spells of shouting, coughing, or vomiting.1,2 The condition is diagnosed when a clear cause (aerodigestive rupture, barotrauma, infection secondary to gas-forming organisms)3 for pneumomediastinum cannot be clearly identified on diagnostic studies. Macklin and Macklin were the first to note the pathogenesis of the syndrome and explained that the common denominator to spontaneous pneumomediastinum was that increased alveolar pressure leads to alveolar rupture.3 Common clinical findings for spontaneous pneumomediastinum include: chest pain, dyspnea, cough, and emesis.4 The condition is not always readily recognized on initial presentation in part for its rare incidence, estimated to be approximately 1 in every 44,500 ED patients3and also because of the non-specific presenting symptoms. For this patient, there was no clear singular cause, and therefore she received care for spontaneous pneumomediastinum.
Hamman’s sign, crepitus heard with auscultation of the chest, is understood to be a more specific indicator of pneumomediastinum.3,4 CT is the ideal diagnostic modality in order to most accurately determine the presence of free air in the mediastinum.3 For this patient, treatment involved symptom management and brief hospitalization for observation purposes. Typical standard of care encourages bed rest with limited physical activity and pain management sometimes also with oxygen administration, anti-anxiety drugs, and cough suppressants, all with the intent to decrease alveolar stress.3 While spontaneous pneumomediastinum may be a more benign condition when ultimately diagnosed, it is important to recognize and seriously consider the differential diagnosis for pneumomediastinum because it includes conditions that demand urgent diagnosis, workup and often definitive treatment.
Topics:
Pneumomediastinum, Hamman’s syndrome, gastric cancer, computerized tomography.
References:
- Dioníio P, Martins L, Moreira S, et al.Spontaneous pneumomediastinum: experience in 18 patients during the last 12 years. J Bras Pneumol.2017;43(2):101-105. doi: 10.1590/S1806-37562016000000052
- Krishnan P, Das S, Bhattacharyya C. Epidural pneumorrhachis consequent to Hamman syndrome. J Neurosci Rural Pract. 2017;8(1):118-119. doi: 10.4103/0976-3147.193525
- Kouritas VK, Konstantinos P, Lazaridis G, et al. Pneumomediastinum. J Thorac Dis.2015;7(Suppl 1):S44–S49. doi: 10.3978/2072-1439.2015.01.11
- Caceres M, Ali SZ, Braud R, et al. Spontaneous pneumomediastinum: a comparative study and review of the literature.Ann Thorac Surg. 2008;86(3):962-66. doi: 1016/j.athoracsur.2008.04.067