A Case Report of Carotid Cavernous Fistula: A Commonly Missed Diagnosis
ABSTRACT:
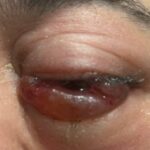
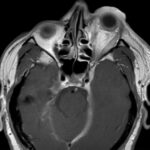
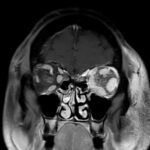
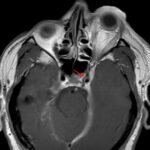
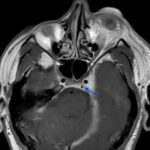
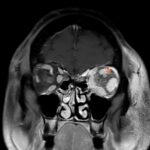
Orbital compartment syndrome (OCS) is an ophthalmologic emergency due to an acute rise in intra-orbital pressure and can result in permanent vision loss, oftentimes requiring emergent surgical decompression. Orbital compartment syndrome most commonly occurs due to recent trauma and is often easily diagnosed by history and physical exam. However, there are other causes of OCS where a more subacute/chronic rise in pressure can lead to an atypical presentation. This is a case report of a 48-year-old male who presented with left eye pain and swelling for the past 6 months. The patient had seen two ophthalmologists prior to his emergency department (ED) presentation who had prescribed him an antibiotic ointment, oral steroids, and steroid eye drops. The physical exam in the ED was concerning for increased intra-ocular pressure (IOP) and decreased vision. Ophthalmology was consulted and requested magnetic resonance angiography (MRA) to assess a vascular etiology given tortuous retinal vasculature. Emergent surgical decompression was deferred due to chronicity of symptoms, and patient was started on dorzolamide/timolol and brimonidine eye drops as well as intravenous (IV) acetazolamide with subsequent improvement in IOP. Imaging revealed a left carotid-cavernous sinus fistula (CCF), and the patient was admitted to neurosurgery. Patient successfully had an embolization with subsequent normalization of IOP and improvement of symptoms. This case is a good example of how non-traumatic causes of OCS can lead to misdiagnosis and how surgical decompression could potentially be deferred in subacute OCS.
Topics: Ocular compartment syndrome, carotid cavernous fistula, eye pain, eye swelling, vision loss.